Authored by Dr. Amber Hayden, DO
You’ve heard the terms “blood sugar” and “blood glucose” but if you’re confused about why they matter, this guide can help.

What is blood glucose?
Blood glucose, also known as blood sugar, is one of the most important sources of energy for your body. When you eat, food is broken down into basic nutrients: fats, proteins, and carbohydrates. Carbohydrates — fiber, starch, and sugar — are broken down into glucose or “blood sugar.”
Glucose is the only fuel used by brain cells except under extreme conditions like starvation. Muscle cells use glucose during short bursts of activity like running to your car in a rainstorm. Having good blood sugar balance is an important benchmark of overall wellness because it prevents certain endocrine imbalances that can threaten your health.
Glucose needs insulin to fuel your cells
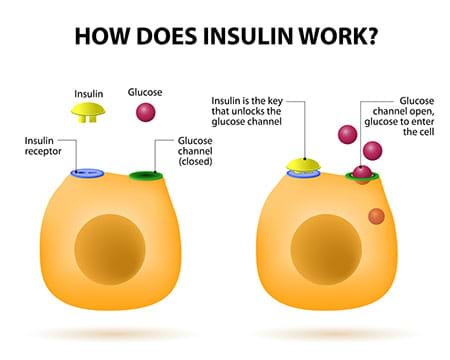
Glucose circulating in your blood needs help to get into the cells. Insulin, a hormone made by the pancreas, is the “key” that turns the “lock” (a cell’s insulin receptor) to let glucose enter. When a cell is working hard — like a muscle cell rapidly expanding and contracting during exercise — it needs more glucose for fuel. So the cell “summons” insulin to bring in more glucose by increasing the number of insulin receptors on its surface. Then insulin can increase the amount of glucose it has to offer the cell as necessary.
Healthy glucose levels are a balancing act
Blood glucose rises and falls in a process called glucose homeostasis. Blood glucose goes up after you eat carbohydrates but it can also increase in response to stress, illness, or even excitement. Rising blood glucose signals the pancreas to release more insulin so blood glucose levels stay in the healthy range. For people without diabetes, that’s around 70 ng/dL (if they haven’t eaten for a while) to about 120 ng/dL .
In addition to getting glucose from digesting carbohydrates, we have backup storage we can turn to. Excess glucose from high-carb meals is converted into glycogen, a complex sugar that’s kept in the liver or converted into fat to use if circulating glucose runs low.
Your body also has a glucose “safety net” if blood glucose falls too low: the pancreas releases glucagon, a hormone that tells the liver to open its energy storehouse and release glycogen. Glycogen gets broken down into glucose and blood sugar rises.
Wonderfully, there’s also back-up for the back-up: fat. When glycogen stores are full, the liver turns excess glucose into fatty acids for storage in fat cells. If you are working really hard, and use up all the glucose as well as stored glycogen, your body breaks down fat cells into glucose, fatty acids and byproducts called ketone bodies. This generally keeps blood glucose levels high enough for your cells to keep working.
What blood glucose testing levels mean
- Normal blood glucose is generally between 70 ng/dL (fasting) and up to 140 (after a meal).
- A fasting blood glucose of 100–119ng/dL means you’re at risk of type 2 diabetes.
- A fasting blood glucose ≥120 or Hemogloblin A1c >6.5% on two occasions, or a non-fasting blood glucose >200, means you have type 2 diabetes.
The spectrum of potential blood sugar problems
Your body’s elegant glucose transfer-and-storage system can go wrong in a number of ways:
- Type 1 diabetes — the immune system sometimes mistakenly attacks pancreatic cells, leaving the pancreas unable to produce insulin, and this happens for various reasons. Without insulin, blood glucose rises to above-normal levels (hyperglycemia).The cells starve without insulin because there’s no way for glucose to get into them —unless insulin is injected. This is also sometimes seen in advanced type II diabetes.
- Insulin resistance — the pancreas makes plenty of insulin but cells stop responding to it. Since glucose can’t get into the cells, it accumulates in the bloodstream. Researchers say insulin resistance is related to several key factors including genetics, diet, exercise level, weight and lifestyle.
- Type 2 diabetes — if a person is insulin resistant (which is primarily due to obesity, poor diet and low activity), the body signals for more and more insulin to pour out of the pancreas to move glucose into the cells. In the long term, this pathway becomes exhausted, and cells are less able to absorb sugar. Eventually the body panics and behaves as if it’s starving. It breaks down fat for energy but that creates a domino effect of elevated blood glucose (hyperglycemia) and circulating fatty acids that end up promoting more insulin resistance. Meanwhile, the excess glucose gets stored in fat cells, or worse, it’s excreted in the urine (glucosuria) — and when that happens, you’ve got type 2 diabetes.
- Hypoglycemia (low blood sugar) — if insulin levels get too high, blood glucose levels go down too fast, leaving you feeling weak, woozy, cranky and craving carbs. Hypoglycemia is a very serious condition that can lead to loss of consciousness.
- Inflammation — this immune system response to stress, illness and toxins can raise blood sugar. If the body needs additional resources to help the immune system, glucose is released by the liver and blood sugar rises. This is fine in the short term but systemic, chronic inflammation degrades the body’s insulin response and leads to bigger problems pretty quickly.

Best practices for healthy blood sugar: what to know about diet, weight and exercise
To have healthy blood sugar levels, you may need to make the following changes in any, or all, of these three areas:
1. Diet
Manage the number of simple carbohydrates you eat every day to cut down on the glucose you’re taking in from food. Even people with diabetes can (and should at certain times) eat some simple carbohydrates. Aim to balance food groups and pair carbohydrates with protein, unsaturated fats, and foods high in fiber like leafy greens.
2. Weight
Keep or find a healthy weight to tamp down inflammation and to increase insulin sensitivity. While it can be very hard to lose weight, find an easy-to-follow plan that allows you to choose your favorite foods in each category. Then you’ll be creating the conditions for steady, healthy weight loss. It’s very important to not skip meals, especially breakfast. Regular meals are essential for maintaining balanced glucose levels and reducing sugar cravings.
3. Activity Level
Exercise helps reduce both inflammation and blood glucose, and makes cells more insulin sensitive. It also reduces stress which helps prevent both inflammation and over-production of stress hormones that raise blood glucose levels. Just 15 minutes can decrease blood glucose levels, even in people with insulin resistance. Your goal should be at least 30 minutes of exercise, 5 days per week. If you exercise before or after a meal, it promotes better insulin sensitivity and glucose usage to further stabilize your blood sugar.
Keeping your blood sugar within healthy limits is one of the most powerful steps to prioritize so you feel your best and stay well. If you’re already dealing with elevated blood sugar, read our article and talk to your doctor about your next steps. You’re ready to feel better and more energetic — aren’t you?
Goodsell, D. (2015). Molecule of the month: Insulin receptor. RCSB PDB-101: doi:10.2210/rcsb_pdb/mom_2015_2 https://pdb101.rcsb.org/motm/182). Accessed 10.19.16.
Boucher, J., Kleinridders, A., and Kahn, C.R. (2014). Insulin Receptor Signaling in Normal and Insulin-Resistant States. Cold Spring Harbor Persp Biol. doi: 10.1101/cshperspect.a009191 (retrieved October 19, 2016 from https://cshperspectives.cshlp.org/content/6/1/a009191.full).
American Diabetes Association. (2013). Living with Diabetes: Stress. https://www.diabetes.org/living-with-diabetes/complications/mental-health/stress.html Accessed 10.19.16.
Colberg, SR, Hernandez, MJ, and Shahzad, F. Blood Glucose Responses to Type, Intensity, Duration, and Timing of Exercise. Diabetes Care 2013 Oct; 36(10): e177-e177. https://dx.doi.org/10.2337/dc13-0965
T. D. Heden, N. C. Winn, A. Mari, F. W. Booth, R. S. Rector, J. P. Thyfault, J. A. Kanaley. Post-dinner resistance exercise improves postprandial risk factors more effectively than pre-dinner resistance exercise in patients with type 2 diabetes. Journal of Applied Physiology, 2014; DOI: 10.1152/japplphysiol.00917.2014