Authored by Dr. Sarika Arora, MD
It’s not unusual for women to develop symptoms of hypothyroidism during perimenopause and menopause — fatigue, intolerance to cold, dry skin, brittle fingernails, itchy scalp, hair loss and stubborn weight gain.

But when women bring these symptoms up, most conventional practitioners take a “wait-and-see” approach rather than recommending any of the nutritional and lifestyle changes that can help support a faltering thyroid. This is especially true if thyroid-stimulating hormone (TSH) levels in your blood work show up as normal or near-normal.
So why doesn’t your doctor help you?
What your doctor doesn’t realize…
I know from experience that you can’t really blame your doctor for not taking action. Doctors in general are trained to use specific tools — and that tool set rarely includes nutrition.
In most medical schools, students cover nutrition for only one day! Even in programs that pay nutrition more than lip service, nutrition may be covered for a few weeks at most.
When I was working in the hospital setting I quickly learned that patients did not see lasting results unless there was a focus on making lifestyle changes. I knew that nutrition needed to be the first step in my therapeutic strategy. So in my case, I specifically chose to further my education after medical school with the Institute for Functional Medicine because it offers a greater focus on nutrition and lifestyle medicine.
As it turns out, the science behind that approach just gets stronger every day. But those doctors who lack knowledge about nutrition are limited in the face of many important health issues. Subclinical hypothyroidism is one of the clearest examples — but unfortunately, just one of many.
Subclinical hypothyroidism is not all in your head
Another issue is your doctor’s approach to diagnosis. If there is no elevated TSH, it’s easy to dismiss all of your problems as related to something other than subclinical hypothyroidism.
For example, there’s a known relationship between sleep apnea and abnormal thyroid hormone levels. But doctors may dismiss fatigue associated with low thyroid function as being due to “poor sleep” without any further investigation. And, of course, poor sleep itself can make all of the cognitive problems worse, too!
The good news for anyone who is frustrated by the lack of answers to their symptoms is that there are proactive steps you can take to solve your thyroid symptoms.
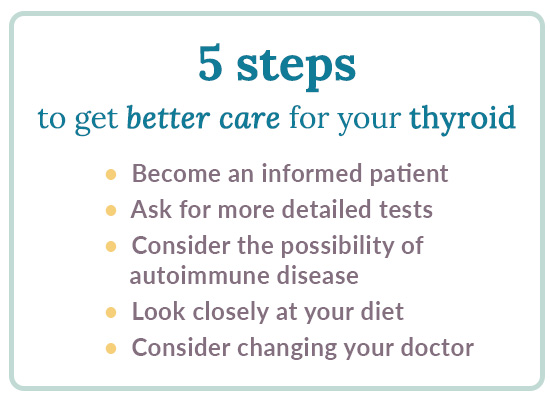
5 steps to get better care for your thyroid
- Become an informed patient. The more you know, the better your health outcomes. You can’t just rely on your doctor to be all-knowing. Conventional practitioners may be smart and well-educated, but they aren’t perfect — and they can only do what they’ve been trained to do.
- Ask for more detailed tests. Most practitioners test TSH, and only TSH. If you’ve had a normal TSH result on a recent test despite experiencing the typical symptoms of low thyroid function, it’s worth getting the full thyroid panel. This includes TSH, free T4, free T3, thyroid peroxidase antibody and thyroglobulin antibody.
- Consider the possibility of autoimmune disease. The most common cause of low thyroid function is Hashimoto’s thyroiditis, an autoimmune disease of the thyroid. If you have autoimmune disorders in your family history, or if you have already been diagnosed with an autoimmune disorder, ask your doctor to test for the anti-thyroid autoantibodies listed above. A positive test is more evidence to convince your healthcare provider to take action and help you support your thyroid function.
- Look closely at your diet. Normal thyroid hormone levels and autoantibody results don’t necessarily mean there isn’t a problem. The thyroid depends on specific nutrients to function well, and it could be that you simply aren’t getting enough of these. Low iodine, selenium and Vitamin D intake are all nutritional deficiencies that can impair thyroid function. Have these levels checked by your medical provider (especially if you live in an area that only gets sunshine for a few months of the year). You may benefit by consulting with a functional medicine nutritionist to see if some or all of these affect you. Our five steps for thyroid symptom relief article is also a good place to start.
- Consider changing your doctor. If you find your current doctor is not willing to work with you on a natural approach, consider consulting with a functional medicine practitioner or naturopath, both of whom are trained to focus specifically on using nutrition, exercise and lifestyle changes to help the body heal itself. These approaches are proven effective with subclinical hypothyroidism.
You are your own best advocate
Most importantly, you deserve to feel your best. This involves surrounding yourself with a team of caring medical professionals who are committed to helping you reach your health goals. If at any point you feel as though you aren’t receiving the care that you need, you have the right to explore other options.
You should not have to spend one week, or one day, or even one minute suffering from bothersome symptoms because your thyroid problems are “subclinical!”
- Baldini IM, Vita A, Mauri MC, et al. Psychopathological and cognitive features in subclinical hypothyroidism. Prog Neuro-Psychopharmacol Biol Psychiatr. 1997;21(6): 925-935.
- Benseñor IM, Nunes MA, Sander Diniz MF, et al. Subclinical thyroid dysfunction and psychiatric disorders: cross-sectional results from the Brazilian Study of Adult Health (ELSA-Brasil). Clin Endocrinol. 2016;84(2):250–256.
- Demartini B, Ranieri R, Masu A, et al. Depressive Symptoms and Major Depressive Disorder in Patients Affected by Subclinical Hypothyroidism: A Cross-sectional Study. J Nervous Mental Dis. 2014;202(8):603–607.
- Harada PHN, Buring JE, Cook NR, et al. Impact of Subclinical Hypothyroidism on Cardiometabolic Biomarkers in Women. J Endocrine Soc. 2017;1(2):113-123.
- Meng Z, Lu L, Fei W, et al. A Worthy Finding: Decrease in Total Cholesterol and Low-Density Lipoprotein Cholesterol in Treated Mild Subclinical Hypothyroidism. Thyroid 2016;26(8): https://doi.org/10.1089/thy.2016.0010 [ePub ahead of print].
- Papaleontiou M, Cappola AR. Thyroid-Stimulating Hormone in the Evaluation of Subclinical Hypothyroidism. JAMA. 2016;316(15):1592-1593.
- Pasqualetti G, Pagano G, Rengo G., et al. Subclinical Hypothyroidism and Cognitive Impairment: Systematic Review and Meta-Analysis. J Clin Endocrinol Metab. 2015;100(11): 4240-4248, https://doi.org/10.1210/jc.2015-2046.
- Petrone A, Mormile F, Bruni G, et al. Abnormal thyroid hormones and non-thyroidal illness syndrome in obstructive sleep apnea, and effects of CPAP treatment. Sleep Med. 2016;23:21-25.
- Resta O, Pannacciulli N, Di Gioia G, et al. High prevalence of previously unknown subclinical hypothyroidism in obese patients referred to a sleep clinic for sleep disordered breathing. Nutr Metab Cardiovasc Dis. 2004;14(5):248-253.
- Rodondi N, den Elzen WP, Bauer DC. Subclinical Hypothyroidism and the Risk of Coronary Heart Disease and Mortality. JAMA. 2010;304(12):1365-1374.
 | Concerned about your thyroid? Take our quiz to determine if you have symptoms of a low thyroid. |












