Authored by Dr. Susan E. Brown, PhD
When conventional doctors diagnose a woman as having osteoporosis or osteopenia, they are likely to prescribe so-called bone-building drugs like Fosamax, Reclast, Forteo, Evenity, Tymols or Prolia. The problem with this approach is that bone drugs should be a last resort for most women with bone health concerns, not a first choice. That’s because changes to diet, exercise and lifestyle often yield better results for bone health with zero negative side effects. This is especially true for women who have never experienced a fracture and whose bone loss is simply a product of menopause.
There is a small percentage of women who will benefit from these drugs as a first line treatment, for a short time. But how do you figure out what you should do? Or what’s best for your mother, your sister or your best friend?
Let’s get into these factors that determine your best course of action for your bone health issue — starting with the arguments against relying on medications.
A system that’s weighted toward drugs
Americans take more physician-prescribed drugs than any other country in the world and by a large margin. The average woman over 65 is taking at least 5 prescription drugs. And studies show that conventional doctors usually don’t spend much time telling their patients about the risks and side effects.
Then there is the fact that quite a few of us get on these medications and never get off them. If we start taking a blood pressure medication when we’re 55, it’s likely we’ll still be on it when we’re 65 or 75. But none of these drugs were ever tested for long-term use in humans before being approved.
Not only is this an expensive habit — it’s bad for our health. Prescription drugs of any kind — even when taken as directed — kill over 125,000 people a year. That’s almost 9% of all deaths in the United States. Depending on whom you ask, each year between 1.5 and 2.2 million people experience serious adverse drug effects. Yet we have little if any idea about the negative health effects of all those drugs in combination — fatigue, blood pressure problems, lowered immune function and so on.
Of course, medications offer many benefits too and save many lives. The question however is, “In your case, do the benefits outweigh the risks?” Doctors call this the risk/benefit ratio. Each drug has its own benefits and risks. However, the overall data doesn’t support the idea that using multiple medications in the long-term improves health. For example, in Europe, doctors prescribe far fewer drugs but the population shows better health outcomes. This is not just in longevity but also in old-age functionality.
Standard osteoporosis treatment goes against U.S. Surgeon General recommendations
Using bone drugs as the first line of osteoporosis treatment illustrates a serious flaw in our medical system. And it goes against the recommendations of the U.S. Surgeon General. In the massive report Bone Health and Osteoporosis, the U.S. Surgeon General created an “Osteoporosis Treatment Pyramid.” It calls for nutrition, exercise and lifestyle interventions to be the first course of action for treating bone loss and bone drugs as the last choice. That is only after searching for the causes of the bone weakness. It’s troubling that doctors ignore these guidelines in favor of going straight to the top of the pyramid and prescribing a bone drug. If doctors aren’t trained in the bottom of the pyramid, they aren’t going to see its value. (See the pyramid for yourself.)
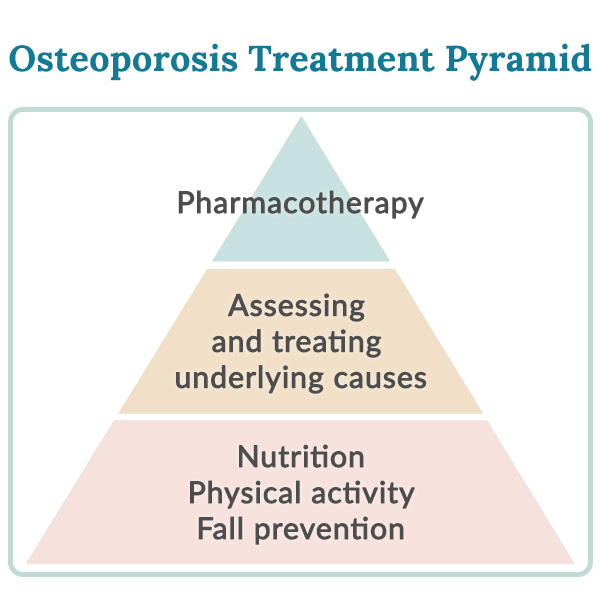
Usually the best prescription for better bones is exercise, a healthy balanced alkaline diet, the reduction of stress and the creation of emotional resilience. The experts know this is true and the studies prove it. In fact, nutrition and weight-bearing exercise are among the universal recommendations in the National Osteoporosis Foundation’s treatment guidelines.
The factors that tip the scales towards a prescription
As a society, we tend to believe that better health comes through chemistry. Physicians prescribe drugs at 73.9% of all office visits. This means that just under three in every four encounters with a doctor result in a pharmaceutical preparation for treatment.
Short doctor visits
Physicians determine that a medication is needed — as well as which medication to choose — based on a very limited amount of time. According to a 2007 study:
- The average doctor’s office visit covers six topics in just over 15 minutes.
- Typically, one of these topics takes up most of the discussion (5 minutes, on average).
- Other topics get only a minute or two for discussion.
Now, suppose you’re seeing your doctor to follow up on the ankle you broke stumbling over a curb. The doctor diagnosed you with osteoporosis after the minor accident. Your physician will take several minutes to examine your ankle and look at x-rays. How long does that leave you to discuss the fact that you have bone weakening? A minute, perhaps two. Can your doctor cram everything there is to know about bone loss, exercise and nutrition into that visit? Hardly! He or she might use those fleeting seconds to suggest you supplement with Vitamin D and calcium. It’s more likely given that you’ve already broken a bone that concern about future fractures will prompt a “magic bullet” approach centering around the osteoporosis go-to prescription: bisphosphonate drugs.
By the time your practitioner is writing the script, their time with you is up. There’s no time for questions about side effects, long-term benefits versus risks or any of the information you might need to make an informed decision about whether this is the right treatment for you. There’s certainly no time to discuss potential options for using nutrition, exercise and other lifestyle changes to help improve your bone health. Although these are well-known for reducing the risk of osteoporotic fractures.
Lack of training in nutrition
The reality is, a majority of physicians lack any significant training in nutrition, even though most of them recognize its importance. Keep in mind that your mainstream conventional doctor is an “allopathic doctor.” This means she/he is trained in the use of drugs, surgery, radiation and chemotherapy to address health symptoms. Most likely this doctor is not trained in nutrition and protocols that would naturally help the body regain balance, bone strength and wellness.
Confusion between bone density and bone weakness
In conventional medicine there persists an overly simplistic understanding of what osteoporosis is and how it develops. There is also a confusion between bone density and bone weakness, which are not the same thing.
It’s understandable to conclude that the thinner bone gets, the weaker it gets. After all, it’s easier to break a single stick between your hands than a thick branch, right? But that’s not always true. A thin willow branch will hold up better to a gale-force wind than a thick oak branch, because it’s flexible and able to bend with the pressure. Similarly, scientific studies have shown that bone quality and structural flexibility, not the total amount or density of bone present, is what most affects your risk of fracture. In many conventional practices, doctors still conflate thinner bone as weaker bone. And a bone drug is prescribed without further assessment.
“Osteopenia” isn’t a real diagnosis
Decades ago, doctors diagnosed osteoporosis only when a patient broke a bone without good reason. For example, say a woman bent over to pick something up and fractured a vertebra as shown by x-ray. It demonstrated that her skeleton was greatly weakened and she received a diagnosis of osteoporosis. This led scientists to wonder whether they could preemptively diagnose osteoporosis by looking at how “dense” the bones were so they could devise a therapy to help avoid these types of fractures. Good intentions, but what happened next made it clear that this was not necessarily well thought out.
Although bone density studies over 35 years document a very weak correlation between fractures and bone density, doctors began to equate the two. They did so without thinking about the fact that they’re not necessarily the same thing (as in our oak versus willow example above).
Worse, when a committee of bone researchers in 1994 came up with a descriptive word, osteopenia, to distinguish women whose bone density was considerably lower than what the researchers considered the norm, it was immediately snatched up as an indicator of disease in need of — you guessed it — a drug. Major researchers themselves argued against this approach because there was no evidence that osteopenia actually did lead to osteoporosis, or that “osteopenia” patients benefited sufficiently from increased bone density to make their drug use worthwhile.
Still, when you get a DEXA and it shows lower bone density, a conventional doctor will likely prescribe a bone drug without doing anything else to assess the strength and flexibility of your bone.
Quantity over quality
And all of this is important because some bone drugs add quantity to bone but reduce quality. Remember, treating the symptom with a drug doesn’t cure the disease — it simply masks the problem. The “problem masking” in turn often brings with it significant life-damaging side effects. Most physicians don’t mention that these are very powerful medications with a profound impact on the body’s most fundamental processes. Long-term bisphosphonate use produces much denser bones but with a greater presence of microscopic cracks. These have the potential to develop into fractures when placed under strain. Denosumab (Prolia) goes even further in interfering with immune factors to prevent the natural process of bone breakdown and renewal. A full 6% of Prolia users will develop a spontaneous vertebral fracture after stopping the drug, unless they immediately start taking a strong bone drug like Reclast to halt bone breakdown.
Profits over health priorities?
Bone drugs are big money makers. The global osteoporosis drug market is currently valued at over $14 billion. It is projected to rise to nearly 23 billion by 2030. Bisphosphonates account for 31% of bone drug prescriptions, roughly $1.25 billion per year in the United States alone. It’s no wonder this huge profit opportunity has shaped the very diagnosis of bone health — in ways that have improved sales but not necessarily patient outcomes.
It’s an unfortunate reality that for the U.S. healthcare system the profit motive has pushed aside consideration of what’s best for individual patients. Over a decade ago, one bioethicist warned that the pharmaceutical industry, which funds a majority of clinical trials, “sets up a research agenda guided more by marketing than by clinical considerations. Smart statistical and epidemiological tactics help obtain the desired results. The budget for marketing is by far greater than for research… By contrast, powerful and cheap health-promoting activities … are markedly underutilized: technologies for changing behavior (e.g., cardiac rehabilitation), palliative care, and use of old, effective, and safe drugs — all could benefit from industry’s tools of marketing and quality.”
How much more is this true today?
So who really needs a prescription drug for bone health?
Let’s face the facts: The reason doctors issue so many prescriptions is because that’s what our healthcare system rewards. If you want a different kind of care for yourself, you need to be proactive. Ask questions, weigh options and above all, learn by researching the things your doctor doesn’t have time to discuss.
If my stance leads you to believe I’m against bone drugs altogether, you need to know that’s not the case. There are people who have such catastrophic bone loss/bone weakening that it’s appropriate for them to use medications to slow or halt it. These are usually people who have a serious ongoing health crisis. That includes patients undergoing cancer treatment, those with Paget’s disease of bone, those on long-term high-dose prednisone treatment or other situations where bone is eroding rapidly. These are clearly circumstances where strong medications can be beneficial, but that’s in addition to supporting bones and overall health with nutrition and life changes.
What it boils down to is this: If your doctor finds your bone health situation so serious that she wants you to take these very powerful drugs — medications that affect not just bones, but other systems in the body too, then your situation is serious enough to warrant a full osteoporosis medical work-up looking for the causes of bone loss! The case for bone drugs cannot be made on the basis of just one or even two DEXAs. In my opinion, the simple fact that a person is losing bone isn’t reason enough to start someone on a drug. Further tests and considerations are needed.
Testing and natural support
My online course, “Osteo Lab Tests: Find Your Hidden Causes” and one of my blogs detail all the tests which should be done when looking into the real causes of excessive bone weakening.
If there is an identifiable underlying condition that is causing an individual to lose a lot of bone rapidly, this should be identified and addressed.
When there isn’t an identifiable underlying health issue or an identifiable cause of bone loss, it stands to reason that working to support bones naturally is a better course of action. Improving nutrient intake, including optimal intake of Vitamin D, magnesium, Vitamin K, calcium and the other key nutrients for bone health (check out my Better Bones Builder for optimal supplementation), exercising for bone health, and making other lifestyle changes are much more sensible first steps.
There must be a very compelling reason to resort to bone drugs and only after careful consideration and investigation.
So that is why I believe your very first question about any medication you’re offered for your bones should be: Is this something I really need to improve my bones?
You deserve the time it takes to get the right answer.











