Authored by Dr. Sarika Arora, MD
I know it can be scary to even think about having a heart attack, but please take a minute to read this. The information here can make a big difference when it comes to saving your life, or that of a loved one.

You may have heard that signs of a heart attack or heart disease for women are different than those for men. But most of us don’t know what the warning signs of a heart attack for women actually are.
Some women suffering from a heart attack may think they just have a bad flu because their symptoms don’t seem anything like a heart attack.
Here are 8 warning signs of a heart attack for women:
If you think you or someone else is having a heart attack, call 9–1–1.
Immediate treatment can save a life or limit the health damage caused by a heart attack.
1. Chest pain
Chest pain is still a top warning signs when it comes to a heart attack for women. But still, some women may not realize they are having a heart attack because the chest pain is so subtle. Other times the pain may feel more like uncomfortable pressure, squeezing, tightness or discomfort in the chest. It can last a few minutes or more, or go away and come back.
2. Shortness of breath
Shortness of breath may occur with or without chest discomfort. Women may be more likely than men to experience this symptom
3. Flu-like symptoms
You may think you have the flu because you’re suffering from chills and cold sweats. Other flu-like symptoms are nausea and lightheadedness, listed below.
4. Nausea and lightheadedness
These symptoms are slightly more common for women than men. Some women may also experience vomiting.
5. Heart palpitations
Your heart rate may increase for no reason.
6. Discomfort in other areas
Pain or discomfort may appear in one or both arms (especially the left arm), the back, between the shoulder blades, neck, jaw or stomach.
7. Heartburn or indigestion
These two symptoms may take place during a heart attack – or up to a month before.
8. Extreme fatigue
Fatigue is a symptom for so many things. If your fatigue is new or extreme, it is worth getting it checked, especially if it happens along with the other symptoms in this list.
What women can do to reduce risk of heart attack
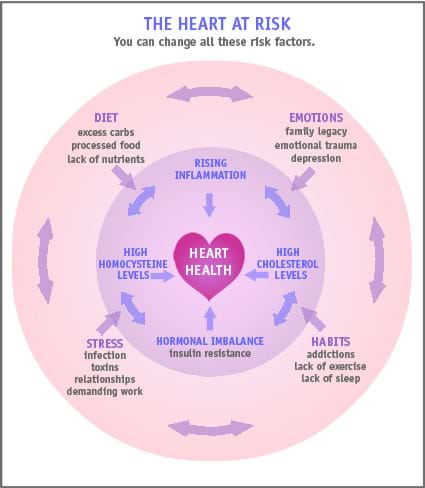
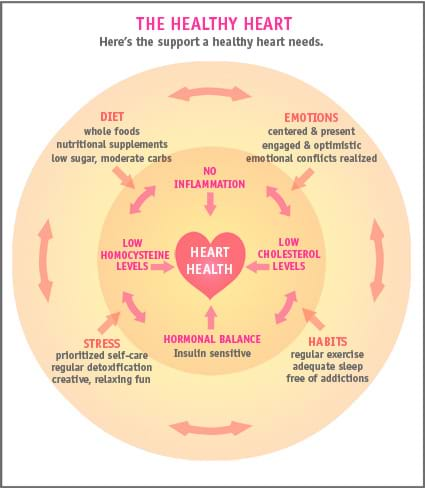
You may already know many of the risk factors for heart disease, such as family history, weight gain around the middle, smoking and high blood pressure. But there are other lesser-known risk factors that are also important. Here’s what to do about them:
- Talk with your practitioner about your inflammation and high homocysteine levels: High homocysteine levels are linked to vascular disorders including heart disease, stroke and peripheral artery disease as well as dementia and Alzheimer’s disease. Elevated homocysteine is specifically associated with thrombosis (blood clots) causing a 2-3 fold increase in risk of cardiovascular events. It is considered as strong of an indicator of vascular disease as smoking or hypertension. The optimal range is for your homocysteine level is 5-8 umol/L. High sensitivity C-reactive protein (hs-CRP) also indicates inflammation. The optimal level is less than 1mg/L.
- Get your cholesterol checked – again: New testing guidelines focus less on only your LDL level (aka the “bad” cholesterol). That’s because a high cholesterol count is not necessarily bad as long as your LDL is low and HDL is high. For LDL, a level of more than 130 mg/dL is considered high risk. For HDL, a level of less than 40 mg/dL is considered high risk.If you have a family history of heart disease, you can have your doctor order an advanced cholesterol panel that will give more information on the LDL-particle number and size.
Even when LDL levels are not in the high-risk range, high levels of Lp (a) and ApoB100 are associated with increased risk of cardiovascular disease. Lp (a) should be under 75 nmol/L. Apolipoprotein B levels should be under 100 mg/dL. Knowing your numbers will guide your doctor to help improve risk assessment.
- Understand if you are pre-diabetic or diabetic you are at significantly increased risk of heart disease. Hemoglobin A1C is used to measure your average blood sugar and to assess for diabetes. A level of less than 5.5% is optimal. A level of 5.7-6.4% indicates you may be pre-diabetic. A level of more than 7% is diagnostic of diabetes.
A note about declining estrogen in menopause. After the age of 55, your risk of heart attack increases greatly, especially if you’ve gone through menopause. This may be because of estrogen’s protective effects on the inner lining of the blood vessels – when estrogen declines, so does the health of the blood vessel walls. But, hormone replacement therapy (HRT) carries risks too. The Women’s Health Initiative showed that both equine-based and synthetic hormone replacement therapies (such as Premarin) increase heart disease risk in postmenopausal women.
You may also notice that other risk factors increase around menopause. This is more likely if you’ve had less than healthy diet and lifestyle habits in the past – and that’s most of us! But remember, you can still do so much to reduce your risk going forward.
One patient’s success story
Carol, 59 years young, had a history of high cholesterol, high blood sugar and low hormones from menopause. We discussed lifestyle medicine and optimized her nutrition plan, adding more phytonutrient dense foods, veggies and decreased sugar. She started working with a personal trainer twice weekly and lost body fat. We rechecked many of the labs discussed above. Her cholesterol decreased and we were able to taper off her statin medication. After a few months, we decreased her metformin. Currently she is completely off both of these medications!She was determined and motivated to decrease her cardiovascular risk and she did it!Carol is delighted that she does not have to take extra medications and that her lifestyle is optimizing her health. We used the concept of epigenetics (environment impacting your genes) and nutrigenomics (food is medicine) to optimize her heart health.
Preventing heart disease with a natural approach
You can start reducing your risk of heart disease right now with the heart-healthy habits found in our article Preventing heart disease – the natural approach. I encourage you to share it with a friend too!
- Varga EA, et al. Cardiology patient pages. Homocysteine and MTHFR mutations: relation to thrombosis and coronary artery disease. Circulation 2005;111:e289-293.
- RavagliaG, et al. Homocysteine and folate as risk factors for dementia and Alzheimer disease.Am J Clin Nutr 2005;82:636-643.
- Hankey GJ, Eikelboom JW. Homocysteine and vascular disease. Lancet 1999;354(9176):407-413.
- Kaptoge S, et al. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet 2009;375:132-140.
- Albert CM, et al. Prospective study of C-reactive protein, homocysteine, and plasma lipid levels as predictors of sudden cardiac death. Circulation 2002:105:2505-2509.
- Prado KB, Shugg S, Backstrand JR. Low-density lipoprotein particle number predicts coronary artery calcification in asymptomatic adults at intermediate risk of cardiovascular disease.
- J Clin Lipidol. 2011 Sep;5(5):408-13. doi: 10.1016/j.jacl.2011.07.001.
- Handbook of Lipoprotein Testing, 2nd Edition, American Association for Clinical Chemistry, Inc. Press, Washington DC, 2000.
- Evaluation of lipoprotein(a) as a prothrombotic factor: progress from bench to bedside. Curr Opin Lipidol. 2003;14(4): pages 361-366.
- Lipoprotein(a)-cholesterol and coronary heart disease in the Framingham Heart Study. Clinical Chemistry. 1999; 45: pages 1039-1046.
- Sniderman et al. A Meta-Analysis of Low-Density Lipoprotein Cholesterol, Non-High-Density Lipoprotein Cholesterol, and Apolipoprotein B as Markers of Cardiovascular Risk. Circ Cardiovasc Qual Outcomes 2011;4:337-345.
- https://www.health.harvard.edu/heart-disease-overview/heart-attacks-in-women