Authored by Dr. Sarika Arora, MD
Endometriosis affects roughly 1 in 10 women of childbearing age worldwide – a distressing number that is only expected to increase. What’s worse, it can take between 4—11 years after symptom onset for a woman to receive an accurate endometriosis diagnosis. Endometriosis has a profound effect on the quality of life for millions of women all over the world. When left untreated, endometriosis can lead to infertility and disrupt a woman’s ability to attend school or work.

Endometriosis is not a condition to ignore, so why is it so difficult to diagnose? And what can women struggling with endometriosis symptoms do to feel better?
Here is what we know about this disease now.
What is endometriosis?
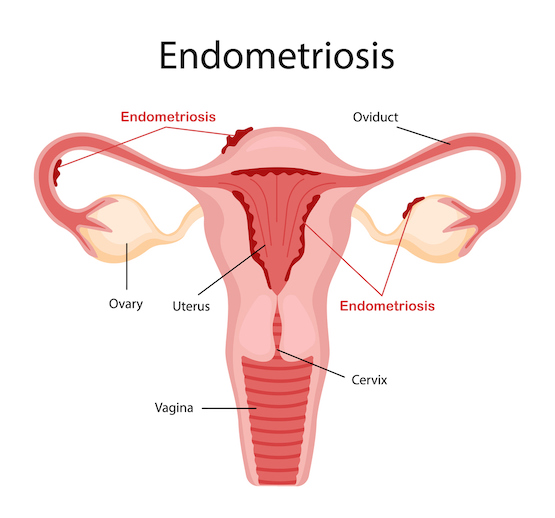
Endometriosis is classified as a chronic inflammatory condition in which the endometrial lining extends beyond the uterus. It causes painful menstrual periods and symptoms that negatively impact daily life. The latest science demonstrates that endometriosis is a hormone-dependent disease. It affects up to 15% of women of child-bearing age, causing 30-50% of those women to experience infertility.
Women with endometriosis may seek out help only after years of suffering. The list of symptoms can be extremely variable, although the most common one is painful periods.
Symptoms of endometriosis
- Painful periods & heavy periods
- Painful sex
- Painful urination or bowel movements
- General pelvic pain or lower back ache
- Bloating
- Nausea
- Infertility
- Fatigue
- Depression
- Anxiety
Painful periods are not normal

Many women report that despite suffering from painful and heavy periods for years, their symptoms are often dismissed or glossed over when they seek medical advice. Unfortunately, there is still a lingering “normalization” of debilitating menstrual symptoms. As a result, many nuances of endometriosis are overlooked. Doctors may prescribe oral birth control pills or hormone replacement therapy (HRT) for heavy/irregular periods or recommend NSAIDs for pain relief, which are not the answer. Let’s be clear: these types of solutions only offer a band-aid approach, masking the real diagnosis.
Limitations of endometriosis diagnostic testing
Currently, invasive laparoscopic surgery is the only conventionally accepted method to diagnose and treat the lesions that indicate endometriosis. This technique is not only invasive, expensive and exhausting — it’s also potentially damaging. More research is needed to develop and test new diagnostic methods, but we’re not there yet.
Even after a successful diagnosis, progression of the disease varies wildly depending on the bio-individuality of a patient and her symptoms. This makes it difficult for doctors to help their patients plan for their futures.
Why do so many women have endometriosis?
The development and widespread use of endocrine-disrupting chemicals — pesticides, herbicides, fungicides, insecticides, PFAS and plastics — over the past 50 years has dramatically changed the way we live and the number of toxins to which we are exposed. Endocrine-disrupting chemicals are more present in our daily environment than ever before. These chemicals behave like xenoestrogens in the body, creating hormonal havoc and the potential for hormonal disorders to develop.

Sadly, the FDA and the EPA have failed to impose regulations to keep consumers safe from exposure. In fact, of 195 countries in the world today, the US holds the #2 spot for highest pesticide use in the world — second only to China. Many of the pesticides that are banned in other nations have increased in usage in the US over the past 10 years.
Many think the health impacts of such heavy toxin exposure are linked to skyrocketing rates of unexplained infertility, hormonal imbalance and endocrine disorders among women, including endometriosis.
Anecdotally, doctors have also seen that women with severe PMS and/or PMDD (premenstrual dysphoric disorder) may be at increased risk for developing endometriosis.
Help for women struggling with endometriosis
If any of the above feels familiar, you might be asking yourself, “What can I be doing right now to help improve symptoms while I wait for a definitive diagnosis?”
While conventional medicine may not have a cure for endometriosis, there is plenty of reason to be hopeful about a future in which women will be able to avoid invasive diagnostic surgery and prevent painful periods.
WHN’s approach to endometriosis
Hormonal imbalance is one of the primary contributing factors to endometriosis. The production and metabolism of female reproductive hormones is a delicate balance. It can be significantly impacted by diet and lifestyle exposures to trans-fats, chemicals, toxins and plastics. This is especially true in younger patients in the early stages of the disease.
For decades, the World Health Organization and the Institute for Functional Medicine have been advocating for long-term diet and lifestyle changes to help maintain hormonal balance. Recommended steps include:
Reducing exposure to toxins
Chemicals and toxins contained in personal care products, pesticides, contaminated water, PFAS in cookware and clothing, and sugars and hydrogenated trans-fats in processed foods are all major endocrine disruptors that can contribute to estrogen dominance and endometriosis.
Food changes
Increased consumption of nutrient-dense foods that help the body detoxify excess estrogens and xenoestrogens, such as broccoli, cauliflower, dark leafy greens, pumpkin seeds, pears, brussel sprouts, kiwi, citrus fruits and bell peppers. Limiting consumption of hydrogenated fats and refined sugars also helps restore hormonal balance.
Address nutrient deficiencies
One study suggests that women with endometriosis had lower vitamin A, C, E, zinc and copper levels compared to women without endometriosis. A 2020 study also found that increased consumption of calcium, magnesium, Vitamin D, B vitamins (especially B6) and select herbal supplements improved PMS symptoms. Both studies found that dietary changes which incorporated these nutrients could significantly alleviate menstrual pain.
Stress support
Stress has been identified as a contributing factor in menstrual irregularities including menorrhagia, oligomenorrhea, dysmenorrhea and PMS – especially in young women. Meditation and mindfulness-based practices can really help. The more we manage our day-to-day stressors, the better we can feel inside. It’s never too late to begin a whole-body approach to your health.
Address estrogen dominance
These days, our bodies are exposed to more external sources of estrogen and stress than our organs can process and detoxify. This results in estrogen dominance, which is a key contributing factor to the build-up of cells in the endometrium — which can lead to endometriosis. Doctors developed our Estrogen Dominance Combo to give your body the targeted nutrient support it needs to detoxify excess estrogen and balance your hormones, without the side effects of conventional HRT or birth control pills.
If you are experiencing signs that something is off, the first step is finding out more about your hormonal health. Take our doctor-developed Hormonal Imbalance Quiz to help understand the scope and severity of your symptoms. If you suspect you might have endometriosis, don’t suffer in silence — early intervention can make all the difference.











