Authored by Caroline Morin, NBC-HWC
We hear a lot about heart health, digestive health and even about brain health, but we don’t often think about how important it is to keep our largest organ, the liver, healthy. Until recently the only perceived danger to the liver was drinking too much alcohol.
“I’m not an alcoholic,” you may be thinking, “so I don’t have to worry about my liver, right?”
The truth is, you probably should worry.
The rise in fatty liver disease
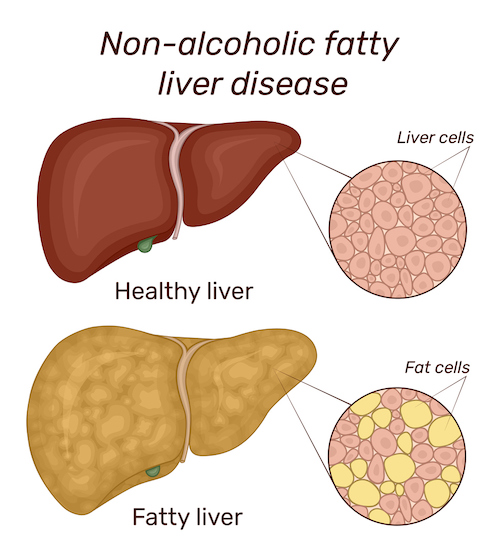
As the standard American diet has changed to include more and more processed foods and sugary drinks, obesity and type 2 diabetes rates have sharply jumped. The same is true for a condition called “non-alcoholic fatty liver disease” (NAFLD). As the name implies, NAFLD is liver dysfunction that involves too much fat stored in liver cells and affects people who drink little to no alcohol.
Over the past 20 years, non-alcoholic fatty liver disease has silently transformed into a major health problem. Today, about 25-30% of adults in the United States and 10% of children between the ages of 2 and 19 have developed fatty liver, and many more people are at risk of developing it.
Despite this prevalence, fatty liver is often completely overlooked as a health concern. So recently, medical experts have started using a more precise name for the condition. They now call it “metabolic dysfunction-associated fatty liver disease” (MAFLD). They’re doing this to make it clearer that this liver condition is closely connected to other health problems, specifically metabolic disorders such as type 2 diabetes. The hope is that by giving it this new name, more people will become aware of the condition, then there will be less misunderstanding or judgment about it.
In this article we’ll learn about the amazing functions our liver performs, how to evaluate your risk for MAFLD and how to manage it — also, better yet, how it’s possible to prevent or reverse fatty liver with simple lifestyle changes.
Here’s what you need to know to start protecting the health of your liver.
Why the health of your liver matters
The liver primarily serves as a filtration system removing toxins and bacteria from over 250 gallons of blood every day. To do so, the liver either breaks down and removes toxins or converts them into something our bodies can safely process.
Added to this important job, the liver performs hundreds of other vital functions involving every system in our bodies. Here are some of the amazing ways the liver takes care of us.
Aids in digestion
All the blood leaving the stomach and intestines passes through the liver. The liver processes and balances nutrients from the food we eat so they can be used by the rest of the body. It also produces bile, which turns fats into energy for the body to use and carries away waste. Bile is necessary for digestion.
Supports hormonal balance
The liver helps to metabolize hormones and remove excess hormones/hormonal metabolites from the body, directly supporting hormonal balance. The liver is the main site for metabolic conversion of estrogens, progesterone and androgens.
Regulates blood sugar
The liver helps your body maintain glucose levels. It supplies glucose to your blood when it needs it, drawing from its store of glycogen. It also removes glucose from your blood when there is too much.
Stores and releases vitamins & minerals
The liver stores vitamins and minerals, particularly iron and copper, and releases them when they are needed in the blood.
Produces substances that help our blood clot
The liver releases plasma proteins that clot our blood.
Controls immune response
The liver removes bacteria therefore helping us to resist infection. Specialized cells in your liver work to detect and destroy harmful viruses, bacteria and other substances in your body, therefore aiding us in resisting infection.
Why is metabolic dysfunction-associated fatty liver disease so common — and how is it harming us?
Dietary trends that began in the 80s, including the prevalence of sugary soft drinks and more access to ultra-processed foods, may explain the rise in diagnosis of fatty liver, not only in America, but globally. High intake of sugar is known to stimulate the liver to produce more fat. So the rise of consumption of high fructose corn syrup starting in the 80s may well have contributed to the rise in fatty liver.
When we consume more calories than we burn, our bodies create additional fat cells to store the surplus energy. From an evolutionary standpoint, this served us well. In times of scarcity, we were able to store energy in these newly created fat cells to use later as a means of survival.
Now that food is so easily accessible and we rarely go more than 12 hours without eating, this evolutionary safety net is no longer needed, and in some cases, if we aren’t careful, it is working against us.
These fat cells can build up anywhere in our bodies. When they build up in the liver, it is called NAFLD, or more recently MAFLD. Generally, people who are overweight are considered to be more at risk for getting fatty liver. But doctors are also discovering that fatty liver is now showing up more and more in people who are not obese.
You can be thin and have fatty liver
In many cases, thin women are developing fatty livers. Doctors believe the rise in diagnosis is a result of a diet high in sugar or processed foods. And surprisingly, fatty liver can be more dangerous for thin people than for those who are overweight. At least one study shows that lean people with fatty liver are more at risk of dying from the disease.
It’s important to note that thin people with non-alcoholic fatty liver disease may have other metabolic disorders including high cholesterol, high blood pressure or type 2 diabetes.
This build up of fat in the liver is not necessarily a problem by itself. But if a fatty liver becomes overburdened with toxins, a virus or bacteria, we are hit with a “double whammy” so to speak. Our now fatty liver cannot perform all the critical functions it is supposed to, and as a result can become inflamed. This is referred to as nonalcoholic steatohepatitis or NASH, and it affects up to 20% of Americans.
This inflammation can lead to further damage in the liver cells including scarring and hardening. Liver disease at this stage is called cirrhosis, something doctors historically only saw in patients with serious alcohol dependency. Cirrhosis can quickly lead to liver failure or liver cancer.
Who’s most at risk?
An astounding 75% of people who are overweight are believed to have NAFLD. But being overweight isn’t the only indicator. Those with other metabolic disorders are even more likely to have fatty liver. You may be at greater risk if you have:
- Cardiovascular disease
- High blood pressure
- High cholesterol
- High triglycerides
- Diabetes or prediabetes
How do I know if I have NAFLD or MAFLD?
You might not know because there are usually no obvious symptoms of a fatty liver. Routine blood work may reveal high liver enzymes which could indicate the disease, but it could go unnoticed.
Be an advocate for your own health by getting regular check ups as well as asking your doctor questions to ensure you understand the results of your blood work.
If you have any of the above risk factors along with high liver enzymes, then your doctor may order an ultrasound or other image testing to get a closer look at the liver to note the extent of the fat buildup.
If diagnosed with NAFLD or MAFLD it is then important to see a hepatologist who specializes in treating the liver.
Supporting a healthy liver

There is no FDA-approved treatment or prescription for fatty liver, but the good news is that, as with other metabolic disorders, lifestyle changes can significantly impact outcomes. Most doctors seem to laud lifestyle modifications as the best course for improving liver health.
Research studies have shown that losing 5-10% of body weight, depending on the progression of the disease, can bring about great improvements. This is a pretty significant amount of weight loss for most folks, but the benefits are great.
Incorporating better nutrition and greater than 150 minutes of moderate exercise each week not only helps improve liver function, it also helps reduce the risk of heart attack and stroke.
Nutrition to support a healthy liver includes:
Fiber
Foods rich in fiber, such as vegetables, fruits and whole grains help reduce inflammation across the body, including the liver. Try apples (with the skin), whole grain brown rice, whole grain oats, beans and berries. Diets high in fiber also promote healthy weight and a reduction of weight supports healing from NAFLD. Women should aim for 21-28 grams of fiber each day.
Cruciferous vegetables
When you eat cruciferous vegetables like broccoli or Brussels sprouts, your stomach acid breaks down a compound in the vegetables called indole-3-carbinol, which then produces a new compound called Diindolylmethane (DIM). DIM plays a role in stimulating natural detoxification enzymes in the liver and also supports normal hormone metabolism, including estrogen metabolism.
Leafy greens
Foods rich in antioxidants help remove free radicals, molecules that can damage your organs, including your liver. Leafy greens like spinach, kale and collards are great sources of antioxidants. They are also packed with fiber, so they have an added bonus.
Lean protein
Lean proteins help you avoid fats that are hard on your liver. Try lean cuts of chicken or fish and avoid or limit red meat.
Fish
Fatty fish like salmon are full of omega-3s which lower inflammation and may lower cholesterol.
Nuts
Walnuts and pecans are full of omega-3s, fiber and antioxidants. Almonds contain Vitamin E which has been shown to aid liver health. Be careful with portion size!
Coffee
Researchers are unsure about why this is, but several studies have shown that coffee may lower your chances of liver cancer and reduce the damage of cirrhosis and other liver diseases. Coffee also contains helpful antioxidants.
Green tea
Green tea has loads of antioxidants. It has been shown to reduce chances of NAFLD. Be sure to enjoy small amounts and avoid the supplements of green tea extract as they have been linked with liver damage.
Stay hydrated
Our bodies are ¾ water and so is our liver. Staying hydrated keeps our bodies balanced and helps our kidneys flush out the toxins.
Herbs and spices
Those included in cooking like oregano, sage, rosemary, cinnamon, garlic, cumin and curry have been shown to be beneficial. As with the green tea, experts recommend enjoying them in their natural form in cooking and not as a supplement.
Reduce alcohol intake
In general women should not have more than a glass a day. Any more puts a burden on the liver. And it’s easy to drink “too much” without being addicted to alcohol. A standard serving is 5 ounces of wine, 12 ounces of beer and 1.5 ounces of liquor. Most glassware holds a lot more than the standard serving size, so it’s easy to accidentally overdo it if you’re not paying attention. Always talk to your doctor about what’s right for you.
Avoid sugar
The liver uses fructose to make fat, so avoiding added sugar is important. Some studies show that sugar is as bad for the liver as alcohol, even if you’re not overweight.
Avoid processed foods
Doctors generally advise to avoid unhealthy fats and processed foods. Avoiding these foods will also support reaching and maintaining a healthy weight.
Making lifestyle changes can be challenging for some people, and receiving a diagnosis like fatty liver can take an emotional toll. Your doctor may be able to recommend a nutritionist or even a health coach to provide further education and support.
A few final tips on taking back the health of your liver
Avoid toxins. Weed killer, pesticides, and even beauty and cleaning products can contain a host of toxins that can overwhelm your liver in its attempts to detox these chemicals from your system. Read and heed warning labels on chemical products you come in contact with — or just skip them altogether! It also helps to carefully wash produce to rinse off any excess herbicides before eating.
Be sure to take medication as prescribed. When the liver is overloaded, it is important to be really careful only to take medication as it is prescribed. Even too much over the counter pain reliever can be problematic.
Talk to your doctor about dietary supplements. If you have fatty liver, check with your doctor before taking anything to make sure it’s safe for your situation. Getting excess amounts of Vitamin A, iron and niacin can be more harmful to someone with NAFLD.
Should I try a liver detox? While it might be tempting to try one of the many liver detoxes on the market, there is not much research on their efficacy. They may interact negatively with an already overloaded liver. Be an informed consumer.
Take charge of your liver health today
Your liver is your body’s unsung hero, performing over 500 vital functions to keep you healthy. However, the rising prevalence of fatty liver disease poses a significant threat to our well-being, regardless of whether you’re overweight or not.
But here’s the good news: You have the power to protect and repair damage to your liver through simple, yet effective lifestyle changes. Your best bet is to make slow and steady positive changes to your diet and exercise, changes you can maintain over time, and to eliminate any potential causes and risk factors. Your liver will thank you.

Don’t wait until symptoms appear; be proactive about your health. Schedule regular check-ups with your doctor, especially if you have risk factors such as cardiovascular disease, high blood pressure, high cholesterol or diabetes. Early detection and intervention can make a world of difference.
Remember, your liver is a resilient organ, and with the right care, you can ensure it continues to perform its vital functions flawlessly. So, prioritize your liver health today.
Start your journey to a healthier liver now, and take control of your future. Don’t wait — act today!
References and further reading
Semmler, G, Datz, C, Reiberger, T, Trauner, M. Diet and exercise in NAFLD/NASH: Beyond the obvious. Liver Int. 2021; 41: 2249–2268.
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, Harrison SA, Brunt EM, Sanyal AJ. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018 Jan;67(1):328-357. doi: 10.1002/hep.29367. Epub 2017 Sep 29. PMID: 28714183.
Perumpail BJ, Li AA, Iqbal U, Sallam S, Shah ND, Kwong W, Cholankeril G, Kim D, Ahmed A. Potential Therapeutic Benefits of Herbs and Supplements in Patients with NAFLD. Diseases. 2018 Sep 10;6(3):80. doi: 10.3390/diseases6030080. PMID: 30201879; PMCID: PMC6165515.
Balakrishnan, Maya MD, MPH Carstensen, Joslyn MPH, RDN, Non Alcoholic Fatty Liver Disease: A Guide of What and How to Eat. The University of Texas Health Science Center at Houston School of Public Health. Baylor Medicine.
Coffee
Kennedy OJ, Roderick P, Buchanan R, Fallowfield JA, Hayes PC, Parkes J. Systematic review with meta-analysis: coffee consumption and the risk of cirrhosis. Aliment Pharmacol Ther. 2016 Mar;43(5):562-74. doi: 10.1111/apt.13523. Epub 2016 Jan 25. PMID: 26806124.
Green Tea
Mahmoodi M, Hosseini R, Kazemi A, Ofori-Asenso R, Mazidi M, Mazloomi SM. Effects of green tea or green tea catechin on liver enzymes in healthy individuals and people with nonalcoholic fatty liver disease: A systematic review and meta-analysis of randomized clinical trials. Phytother Res. 2020 Jul;34(7):1587-1598. doi: 10.1002/ptr.6637. Epub 2020 Feb 18. PMID: 32067271.
Nuts
Chen BB, Han Y, Pan X, Yan J, Liu W, Li Y, Lin X, Xu S, Peng XE. Association between nut intake and non-alcoholic fatty liver disease risk: a retrospective case-control study in a sample of Chinese Han adults. BMJ Open. 2019 Sep 4;9(9):e028961. doi: 10.1136/bmjopen-2019-028961. PMID: 31488477; PMCID: PMC6731785.
Omega 3
Lu W, Li S, Li J, Wang J, Zhang R, Zhou Y, Yin Q, Zheng Y, Wang F, Xia Y, Chen K, Liu T, Lu J, Zhou Y, Guo C. Effects of Omega-3 Fatty Acid in Nonalcoholic Fatty Liver Disease: A Meta-Analysis. Gastroenterol Res Pract. 2016;2016:1459790. doi: 10.1155/2016/1459790. Epub 2016 Aug 29. PMID: 27651787; PMCID: PMC5019889.
Metabolic-associated liver disease
Gill MG, Majumdar A. Metabolic associated fatty liver disease: Addressing a new era in liver transplantation. World J Hepatol. 2020 Dec 27;12(12):1168-1181. doi: 10.4254/wjh.v12.i12.1168. PMID: 33442446; PMCID: PMC7772736.
Lean patients and fatty liver
Wijarnpreecha, K, Li, F, Lundin, SK, Suresh, D, Song, MW, Tao, C, et al. Higher mortality among lean patients with non-alcoholic fatty liver disease despite fewer metabolic comorbidities. Aliment Pharmacol Ther. 2023; 57: 1014–1027.












