Authored by Dr. Sharon Stills, NMD
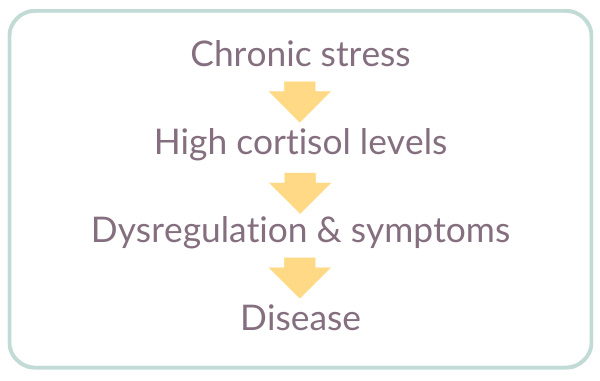
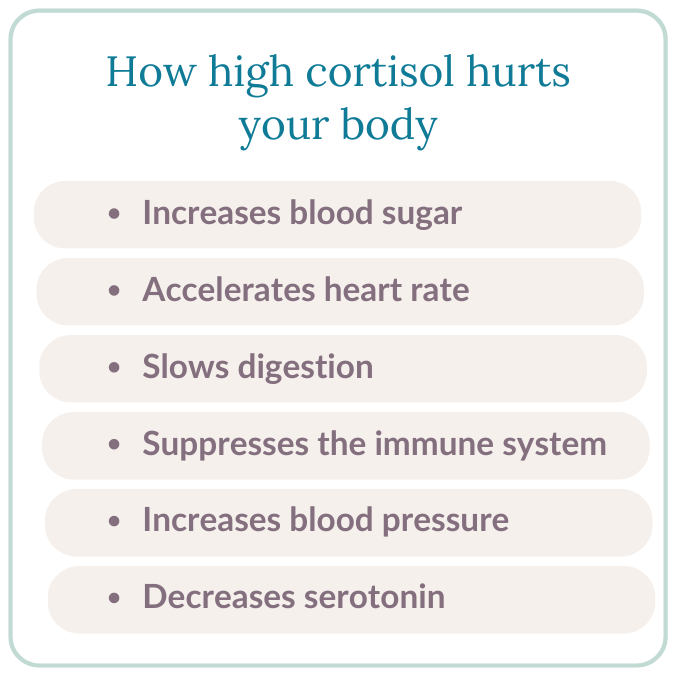
If you have chronic high cortisol it’s almost impossible to balance your other hormones. Excess cortisol is not just a matter of discomfort, either. Over time, chronic high cortisol can lead to a variety of diseases such as cancer, heart disease and Alzheimer’s. Fortunately, we’re not helpless. Let’s talk about what you can do about excess cortisol.
Table of contents
What is cortisol?
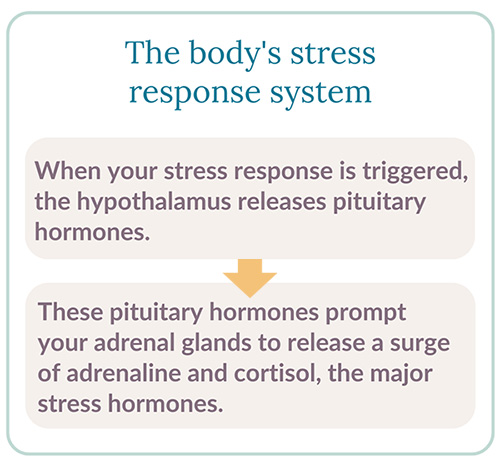
Cortisol is one of the body’s main stress hormones. When you are under stress and your body’s fight or flight response kicks in, cortisol quickly comes to your rescue by mobilizing carbohydrates and fat for instant energy. But even when you’re not in danger, cortisol hums along in the background assisting your body with key everyday functions.
High cortisol signs and symptoms in women
When cortisol production is balanced, levels of the hormone naturally rise and fall during the day. These patterns are tightly connected to your circadian rhythm sleep/wake cycle.
Cortisol levels are usually lowest between midnight and 4 a.m. Then they gradually increase until around 8 a.m. Eventually, rising cortisol helps you to wake up and start the day. Then, after 8 a.m., cortisol declines incrementally throughout the day to gradually prepare you for sleep.
This daily rhythm is the norm — unless you encounter a stressful event. Then your body temporarily raises levels of cortisol and adrenaline to handle the stressful event. Eventually when the stressors have passed, cortisol and adrenaline levels return to normal.
That’s the way it’s supposed to work. Yet when chronic stress leads to unnaturally high cortisol levels, it creates a state of adrenal imbalance that often triggers a cascade of adrenal-related symptoms:
- Insomnia
- Weight gain
- Fatigue
- Brain fog
- Low sex drive
- Sleeplessness
- Weight gain (especially belly fat)
- Impaired healing and cell regeneration
- Disrupted digestion, mental function (brain fog) and metabolism
- Weakened ability to fight infection
- Imbalances in other important hormones such as DHEA, estrogen, progesterone and testosterone
- Loss of muscle and bone
- Mood swings and depression
- Hair and skin problems
- Thyroid imbalances
High cortisol + adrenal fatigue
Adrenal imbalance in women tends to peak between the ages of 35 and 55 and most often shows up in one of the following ways:
- You’re always active and feel “wired.” Your system is constantly fueled by adrenaline and cortisol so it feels like a continual state of hyper-energy. However, you often feel drained.
- You can’t get up in the morning, but you can’t sleep at night. Your natural 24-hour cycle of energy and relaxation is off-balance. If you’re able to fall asleep, you may wake up in the middle of the night fully alert.
- You have no energy — period. You feel exhausted all the time. So even getting out of bed often feels like a challenge. You may also experience intense cravings and unexplained weight gain.
Adrenal imbalance may be a factor in many other serious conditions. For example, fibromyalgia, hypothyroidism, chronic fatigue syndrome, depression, arthritis, anxiety at night and more can result.
Lab testing for high cortisol levels
Unfortunately, conventional tests for adrenal function aren’t very helpful. Typical lab cortisol tests only identify the most severe cases of cortisol dysfunction after they have progressed to a full-blown disease state, such as Addison’s Disease or Cushing’s Disease. But you may be able to find a practitioner willing to do salivary cortisol testing, which measures a hormone called DHEA (dehydroepiandrosterone) throughout the day. But these tests aren’t perfect, either.
Absent a disease state, you can gain useful insight into your cortisol “curve” by watching your own symptoms throughout the day. Pay attention to your body. If your energy level is very low in the morning but seems to increase around the time everyone else is going to bed, your cortisol cycle is dysregulated. This is a good indication that you will reap huge benefits by taking steps to rebalance your adrenal glands.
How to lower cortisol and relieve adrenal fatigue
In our experience, women with mild to moderate adrenal imbalance have several options that can help them feel significantly better while keeping symptoms from becoming more severe.
The key is taking the right steps to normalize cortisol levels and restore healthy adrenal function. You can take immediate action by asking yourself these simple questions:
Are you eating in tune with your natural cortisol curve?
- When you eat your meals is just as important as what you eat to rebalance your adrenal glands. The goal is to achieve more stable energy levels throughout the day, which you can accomplish by eating three balanced meals with two snacks.
- What you eat does make a difference too! Try to reduce refined carbohydrates — such as sugar, flour, potatoes and white rice — which cause stressful ups and downs in your blood sugar that can lead to adrenal imbalance. We know this can be difficult, so just do the best you can. The goal is progress, rather than perfection!
How can nutritional supplements support your adrenal glands?
- High-quality vitamins and minerals help support a healthy metabolism and hormonal balance, which contribute to adrenal health. Our Essential Nutrients, with 30 vitamins and minerals, is an easy-to-take formulation that builds a strong nutritional foundation.
- Specific herbal supplements, such as astragalus root and eleuthuro (Siberian ginseng), are effective at reducing the negative side effects of stress. Others, such as passionflower, produce calming effects and encourage sleep. Many of these herbs are found in our natural formulations Adaptisol and Serinisol.
Which lifestyle changes are best to restore adrenal balance?
- We can’t always reduce stress, but we can take steps to reduce its effects on our lives. Take time to understand where your stress is coming from, and then think about how you’ll make changes that are right for you and your lifestyle. It’s helpful to make a list of stressors that interfere with your well being, especially those that are ongoing or self-imposed.
- Get more rest. Your body needs down time to heal! Aim for at least 7-8 hours a night. So be in bed and sleeping by 10 or 10:30 p.m. at the latest. If you need to unwind, or it takes you a little bit to fall asleep, then get to bed at 9 or 9:30 p.m.
- Get more gentle. Choose forms of physical exercise that calm you down instead of rev you up. For example, walking, yoga, Tai Chi and other forms of low impact exercise can do wonders for the adrenals. On the other hand, high intensity exercise can trigger cortisol production. So listen to your body. If a certain form of exercise makes you feel worse instead of better, move on and try something else.
Remember, it took a lot of time for high cortisol levels to develop so it’s going to take time to bring your adrenals back to balance. Above all, as you work towards this goal, be kind to yourself, be proactive about all the many changes you can make and steps you can take — and know that you will be well again!
References and further reading
Hyman, M. 2005. Chapter 26. Clinical approaches to environmental inputs, 357. In Textbook of Functional Medicine. Gig Harbor, WA: Institute for Functional Medicine.
Williams, G., & Dluhy, R. 2005. Chapter 321. Disorders of the adrenal cortex, 2127–2130. In Harrison’s Principles of Internal Medicine, 16th Edition. NY: McGraw–Hill.
McEwan, B. 2006. Protective and damaging effects of stress mediators: Central role of the brain. Dialogues Clin. Neurosci., 8 (4), 367–381. (accessed 07.07.2010).
Head, K., & Kelly, G. 2009. Nutrients and botanicals for treatment of stress: Adrenal fatigue, neurotransmitter imbalance, anxiety, and restless sleep. Alt. Med. Rev., 14 (2), 114–140. (accessed 07.07.2010).
Wilson, J. 2001. Adrenal Fatigue, the 21st Century Stress Syndrome, 268–273. Petaluma, CA: Smart Publications.
Lawnson, E., et al. 2009. Hypercortisolemia is associated with severity of bone loss and depression in hypothalamic amenorrhea and anorexia nervosa. J. Clin. Endocrinol. Metab., 94 (12), 4710–4716. (accessed 07.06.2010).
Sbaihi, M., et al. 2009. Cortisol mobilizes mineral stores from vertebral skeleton in the European eel: An ancestral origin for glucocorticoid-induced osteoporosis? J. Endocrinol., 201 (2), 241–252. (accessed 07.06.2010).
Sivamani, R., et al. 2009. Stress-mediated increases in systemic and local epinephrine impair skin wound healing: Potential new indication for beta blockers. PLoS, 6 (1), e12. (accessed 07.07.2010).
Head, K., & Kelly, G. 2009.
Scherrer, U., & Sartori, C. 1997. Insulin as a vascular and sympathoexcitatory hormone. Circulation, 96, 4104–4113. (accessed 07.07.2010).
Beluche, I., et al. 2010. A prospective study of diurnal cortisol and cognitive function in community-dwelling elderly people. Psychol. Med., 40 (6), 1039–1049. (accessed 07.07.2010).
Hays, B. 2005. Chapter 19. Hormonal imbalances: Female hormones: The dance of the hormones. Pt. I, 229. In Textbook of Functional Medicine. Gig Harbor, WA: Institute for Functional Medicine.
McEwan, B. 1998. Protective and damaging effects of stress mediators. NEJM, 338 (3), 171–179. (accessed 07.07.2010).
Wilson, J. 2001. Adrenal Fatigue, the 21st Century Stress Syndrome, 290. Petaluma, CA: Smart Publications.
Hardy, R., & Cooper, M. 2010. Adrenal gland and bone. Arch. Biochem. Biophys., 503 (1). 137–145. (accessed 07.07.2010).
Isales, C., et al. 2010. ACTH is a novel regulator of bone mass. Ann. NY Acad.Sci., 1192 (1), 110–116. (accessed 07.07.2010).
Riva, R., et al. 2010. Fibromyalgia syndrome is associated with hypocortisolism. Int. J. Behav. Med. [Epub ahead of print.] (accessed 07.07.2010).
Hays, B. 2005. 229–230.
Zarković, M. 2003. [Disorder of adrenal gland function in chronic fatigue syndrome.] Srp. Arh. Celok. Lek., 131 (9–10), 370–374. (accessed 07.07.2010).
Scott, L., et al. 2000. A preliminary study of dehydroepiandrosterone response to low-dose ACTH in chronic fatigue syndrome and in healthy subjects. Psychiatry Res., 97 (1), 21–28. (accessed 07.07.2010).
Hays, B. 2005. 228–229.
Cutolo, M., et al. 2006. Circadian rhythms: Glucocorticoids and arthritis. Ann. NY Acad. Sci., 1069, 289–299. (accessed 07.07.2010).
Harbuz, M., et al. 2003. Hypothalamo-pituitary-adrenal axis and chronic immune activation. Ann. NY Acad. Sci., 992, 99–106. (accessed 07.07.2010).
Arlt, W., & Allolio, B. 2003. Adrenal insufficiency. Lancet, 361 (9372), 1881–1893. (accessed 07.06.2010).
Oelkers, W. 1996. Adrenal insufficiency. NEJM, 335 (16), 1206–1212. (accessed 07.06.2010).
Al-Qarawi, A., et al. 2002. Liquorice (Glycyrrhiza glabra) and the adrenal-kidney-pituitary axis in rats. Food Chem. Toxicol., 40 (10), 1525–1527. (accessed 07.06.2010).