
Authored by Dr. Mary James, ND
One of the best ways to support your thyroid function is to eat a healthy thyroid diet. Your food choices are especially important during stressful times or hormonal changes – when you are more vulnerable to thyroid problems.
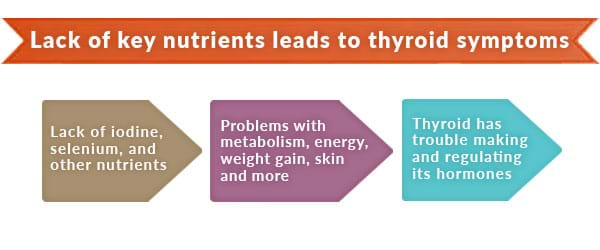
To do its job and keep you symptom-free, the thyroid requires an adequate amount of specific vitamins and minerals from foods. Iodine and selenium are the most important of these nutrients. But trace minerals, antioxidants and B vitamins are also critical for healthy thyroid function. While it’s possible to get too many of these nutrients, which can also cause problems, getting too few of them is more common.
7 nutrients you need to improve thyroid function
1. Iodine
Your thyroid simply can’t function without iodine. If you’re deficient, your thyroid lacks a basic building block for producing its hormones – so your whole body is affected.
Top food sources for iodine:
- Sea vegetables (kelp, dulse, hijiki, nori)
- Seafood (clams, shrimp, haddock, oysters, salmon, sardines)
- Iodized salt, preferably sea salt
In addition to the top food sources, there are good secondary sources: eggs, asparagus, lima beans, mushrooms, spinach, sesame seeds, summer squash, Swiss chard and garlic.
2. Selenium
Selenium is essential to the thyroid because it’s used to convert T4 into T3, the most active form of thyroid hormone. Iodine and selenium are closely related, so a deficiency in selenium can lead to an iodine deficiency.
Top food sources for selenium:
- Brazil nuts
- Tuna
- Organ meats
- Mushrooms
- Halibut
- Beef
- Soybeans
- Sunflower seeds
3. Zinc
Since zinc is required for the conversion of T4 to T3, a deficiency can result in hypothyroidism. Not getting enough zinc, copper or iron causes an imbalance in the other two. So it’s important that you get enough of all 3 of these companion nutrients.
Top food sources for zinc:
- Fresh oysters
- Sardines
- Beef
- Lamb
- Turkey
- Soybeans
- Split peas
- Whole grains
- Sunflower seeds
- Pecans
- Brazil nuts
- Almonds
- Walnuts
- Ginger root
- Maple syrup
4. Copper
Copper is also needed for the conversion of T4 to T3, so low levels can contribute to low thyroid function.
Top food sources for copper:
- Beef
- Oysters
- Lobster
- Shiitake mushrooms
- Dark chocolate
- Crabmeat
- Tomato paste
- Pearled barley
- Nuts
- Beans (soybeans, white beans, chickpeas)
- Sunflower seeds
5. Iron
Research shows a link between iron-deficiency anemia and decreased thyroid function. Low iron can also prevent iodine from working effectively for the thyroid, while too much iron can also be a health problem. So it’s good to get levels checked if you’re not sure.
Top food sources for iron:
- Clams
- Oysters
- Organ meats
- Soybeans
- Pumpkin seeds
- White beans
- Blackstrap molasses
- Lentils
- Spinach

6. Antioxidants
Oxidative stress or inflammation from free radicals is associated with degenerative diseases, as well as the aging process.
Antioxidants such as vitamins A, C and E, along with iodine and selenium, are particularly important because they help your thyroid gland neutralize daily oxidative stress.
Top food sources for vitamins A, C and E:
| Vitamin A (beta-carotene form) | Vitamin C | Vitamin E |
| Kale Sweet potatoes Carrots Winter squash/pumpkin Spinach Cantaloupe Broccoli Asparagus Liver Lettuce | Guava Peppers (chili, bell, sweet) Kiwi Citrus fruit Strawberries Broccoli Cauliflower Brussels sprouts Papaya Parsley Greens (kale, turnip, collard, mustard) | Whole grains Almonds Soybeans Beans Sunflower seeds Peanuts Liver Leafy green vegetables Asparagus |
7. B vitamins
Several B vitamins (B2, B3, and B6) are important for thyroid function because they are involved in manufacturing T4.

Top food sources for vitamins B2, B3 and B6:
| Vitamin B2 (Riboflavin) | Vitamin B3 (Niacin) | Vitamin B6 (Pyridoxine) |
| Organ meats Almonds Wheat germ Wild rice Mushrooms Egg yolks Brewer’s yeast Vitamin B3 | Rice bran Wheat bran Peanuts (with skin) Liver Poultry (white meat) Brewer’s yeast Vitamin B6 | Sunflower seeds Wheat germ Fish (tuna, salmon, trout) Liver Soybeans Beans (lentils, lima, navy, garbanzos, pinto) Walnuts Brown rice Bananas Brewer’s yeast |
What foods should you avoid for good thyroid function?
Certain foods contain goitrogens, which are compounds that make it more difficult for the thyroid gland to create its hormones. For example, soybeans, broccoli, cauliflower, cabbage and Brussels sprouts are goitrogens. But there’s no need to cut these foods out of your diet completely. Instead, we recommend you cook these foods to reduce their goitrogenic properties instead of eating them raw. Another idea is to pair these foods with the thyroid-healthy foods listed above.
One food you may want to avoid is gluten: Many women tell us when they remove gluten-containing foods from their diet, they feel much better and notice fewer problems with their thyroid, especially autoimmune thyroid disease. Learn more about goitrogens, gluten and thyroid health.
Getting enough of the right nutrients
Getting as many thyroid-supporting nutrients as possible through foods is ideal, but this isn’t always easy or even possible. If you tend to grab quick meals while standing at the kitchen counter, eat while driving or in front of a computer on a regular basis, consider supplementing with thyroid-supporting ingredients.
If you already have a diagnosed thyroid imbalance, talk to your practitioner about possibly using supplements before taking prescription hormones. The problem with prescriptions like Synthroid (levothyroxine, or T4) is that once you go on them, your thyroid backs down its efforts to produce hormones. This can make it difficult to get off of thyroid replacement drugs down the line. It’s also possible to use a supplement as “adjunct” therapy alongside prescription medications — many women report good results with this protocol.
1 Kosova, W., & Wingert, P. 2009. Live your best life ever! Why health advice on “Oprah” could make you sick. Newsweek. URL: https://www.newsweek.com/id/200025/page/4(accessed 06.19.2009).
2 Thyroid disease << Frequently asked questions << womenshealth.gov. URL: >https://www.womenshealth.gov/faq/thyroid-disease.cfm (accessed 05.12.2009).
3 Caldwell, K., et al. 2005. Urinary iodine concentration: United States National Health and Nutrition Examination Survey. Thyroid, 15 (7), 692-699. URL: https://www.ncbi.nlm.nih.gov/pubmed/16053386 (accessed 05.12.2009).
4 De la Vieja, A., et al. 2000. Molecular analysis of the sodium/iodide symporter: Impact on thyroid and extrathyroid pathophysiology. Physiol. Rev., 80 (3), 1083–1105. URL: https://physrev.physiology.org/cgi/content/full/80/3/1083 (accessed 05.12.2009).
5 Caldwell, K., et al. 2005. Urinary iodine concentration: United States National Health and Nutrition Examination Survey. Thyroid, 15 (7), 692–699. URL: https://www.ncbi.nlm.nih.gov/pubmed/16053386 (accessed 05.12.2009).
6 Arem, R. 1999. The Thyroid Solution, 302. NY: Ballantine Books.
7 Robin, C. 2007. Iodine Remedies: Secrets from the Sea, 36. Madison, WI: Service to the Good of Life. URL (PDF): https://www.jcrows.com/MaryJoFahey_IodineRemediesSecretsFromTheSea.pdf (accessed 05.18.2009).
Arthur, J., & Beckette, G. 1999. Trace elements and thyroid function. Br. Med. Bull., 55 (3), 658–668. URL: https://bmb.oxfordjournals.org/cgi/reprint/55/3/658 (accessed 05.13.2009).
Sterling, K. 1979. Thyroid hormone action at the cell level. NEJM, 300 (3), 117–123. URL (subscription required): https://www.nejm.org/doi/pdf/10.1056/NEJM197901183000304 (accessed 05.13.2009).
8 Olivieri, O., et al. 1995. Low selenium status in the elderly influences thyroid hormones. Clin. Sci. (Lond.), 89 (6) 637–642. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/8549083 (accessed 05.19.2009).
9 Arem, R. 1999, p. 302.
10 Kandhro, G., et al. 2009. Effect of zinc supplementation on the zinc level in serum and urine and their relation to thyroid hormone profile in male and female goitrous patients. Clin. Nutr., 28 (2), 162–168. URL: https://www.ncbi.nlm.nih.gov/pubmed/19250719 (accessed 05.18.2009).
11 Farooqi, L., et al. 2000. Effects of a single venous dose of zinc on thyroid status in healthy individuals and patients with Graves’ disease. Met.-Based Drugs, 7 (3), 151–155. URL (PDF): https://www.pubmedcentral.nih.gov/picrender.fcgi?artid=2365210&blobtype=pdf (accessed 05.18.2009).
Pekary, A., et al. 1993. Testosterone increases TRH biosynthesis in epididymis but not heart of zinc-deficient rats. Peptides, 14 (2), 315. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/8483808 (accessed 05.18.2009).
Morley, J., et al. 1980. Zinc deficiency, chronic starvation, and hypothalamic-pituitary-thyroid function. Am. J. Clin. Nutr., 33 (8), 1767–1770. URL: https://www.ajcn.org/cgi/reprint/33/8/1767 (accessed 05.18.2009).
12 Kandhro, G. et al. 2008. Evaluation of iron in serum and urine and their relation to thyroid hormone profile in female goitrous patients. Biol. Trace Elem. Res., 125 (3), 203–212. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/18568296 (accessed 05.19.2009).
13 Puckett, C. 2004. Copper and cardiovascular health. Original Internist. URL: https://findarticles.com/p/articles/mi_m0FDL/is_4_11/ai_n17208767/ (accessed 05.06.2009).
Guyton, A., & Hall, J. 2005. Textbook of Medical Physiology, 860. Philadelphia: Saunders.
14 Puckett, C. 2004.
15 Mayo Clinic Staff. 2009. Graves’ disease. Definition. https://www.mayoclinic.com/health/graves-disease/DS00181 (accessed 10.06.2010).
Norman, J. 2010. Hyperthyroidism: Overactivity of the thyroid gland. Part 2: Causes of hyperthyroidism. URL: https://www.endocrineweb.com/conditions/hyperthyroidism/hyperthyroidism-overactivity-thyroid-gland-1 (accessed 10.06.2010).
16 Arem, R. 1999, 302.
Asayama, K., & Kato, K. 1990. Oxidative muscular injury and its relevance to hyperthyroidism. Free Radic. Biol. Med., 8 (3), 293–303. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/2187767 (accessed 05.20.2009).
17 Pizzorno, L., & Ferril, W. 2005. Chapter 32. Clinical approaches to hormonal and neuroendocrine imbalances. Thyroid. In Textbook of Functional Medicine, ed. D. Jones & S. Quinn, 647. Gig Harbor, WA: Institute for Functional Medicine.
18 Kosova, W., & Wingert, P. 2009.
19 Divi, R., et al. 1997. Anti-thyroid isoflavones from soybean: Isolation, characterization, and mechanisms of action. Biochem. Pharmacol., 54 (10), 1087–1096. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/9464451 (accessed 10.06.2010).
Divi, R., & Doerge, D. 1996. Inhibition of thyroid peroxidase by dietary flavonoids. Chem. Res. Toxicol., 9 (1), 16–23. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/8924586 (accessed 10.06.2010).
20 Doerge, D., & Sheehan, D. 2002. Goitrogenic and estrogenic activity of soy isoflavones. Environ. Health Perspect., 100 (Suppl. 3), 349–353. URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1241182/?tool=pubmed (accessed 10.06.2010).
21 Bruce, B., et al. 2003. Isoflavone supplements do not affect thyroid function in iodine-replete postmenopausal women. J. Med. Food, 6 (4), 309–316. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/14977438 (accessed 05.20.2009).
Teas, J., et al. 2007. Seaweed and soy: companion foods in Asian cuisine and their effects on thyroid function in American women. J. Med. Food, 10 (1), 90–100. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/17472472 (accessed 05.20.2009).
22 Pizzorno, L., & Ferril, W. 2005. Chapter 32. Clinical approaches to hormonal and neuroendocrine imbalances. Thyroid. In Textbook of Functional Medicine, ed. D. Jones & S. Quinn, 647. Gig Harbor, WA: Institute for Functional Medicine.
References for text box: What does active thyroid hormone do?
a Carillo Sepulveda, M., & Morais Barreto de Chaves, M. 2008. Nongenomic effects of T3 on NO production in vascular smooth muscle cell (VSMC). FASEB, 22 (1), 965.15. URL (abstract): https://www.fasebj.org/cgi/content/meeting_abstract/22/1_MeetingAbstracts/965.15 (accessed 05.12.2009).
b Seifter, J., et al. 2005. Concepts in Medical Physiology, 532–534. NL: Wolters Kluwer Health. URL: https://books.google.com/books?id=A8H_9S4E0I4C&pg=PA532&lpg=PA532&dq=where+are+there+t4+receptors+in+the+body&source=bl&ots=PmZIyGEFiR&sig=xsNcJcInzFKT-gpB4bzWUCVcBGk&hl=en&ei=oNEJStOSIs-wmAfX-oXjCw&sa=X&oi=book_result&ct=result&resnum=6 (accessed 05.12.2009).
c Weinstein, S., et al. 1994. Thyroid hormone increases basal and insulin-stimulated glucose transport in skeletal muscle. The role of GLUT4 glucose transporter expression. Diabetes, 43 (10), 1185–1189. URL (abstract): https://diabetes.diabetesjournals.org/cgi/content/abstract/43/10/1185 (accessed 05.12.2009).










