Authored by Dr. Sarika Arora, MD
Pelvic floor strengthening with Kegel exercises and other methods is an important part of women’s health — and it has lots of benefits. At least 7 out of 10 women have disorders of the pelvic floor that can be vastly improved with pelvic floor strengthening exercises and other options.

Symptoms of a weakened pelvic floor
When the pelvic muscles can’t properly support a woman’s organs, it can cause problems like these:
- Urinary or stool incontinence
- Constipation or incomplete bowel or bladder emptying
- Diminished sexual satisfaction
- Painful intercourse
- Inability to reach orgasm
- Sagging or prolapse of the uterus, bladder or rectum
- Low back or lower abdominal pain
Many women think that pelvic floor strengthening is only needed after pregnancy and childbirth. But a weakened pelvic floor can affect women of any age, causing distressing symptoms like frequent urination or pain during sex.
Whether you’re already having pelvic floor issues or want to avoid problems later, adding Kegel exercises and other pelvic floor strengthening to your routine can make all the difference.
Take a look at Kegel exercises and other pelvic floor strengthening exercises now.
What is the pelvic floor?
The pelvic floor consists of muscles and ligaments that work like a hammock to hold and support your lower organs. It also:
- Creates the structure for the abdominal cavity and its muscles and organs
- Controls the passage of urine and stool
- Facilitates the childbirth process
- Contributes to sexual pleasure and ability to reach orgasm
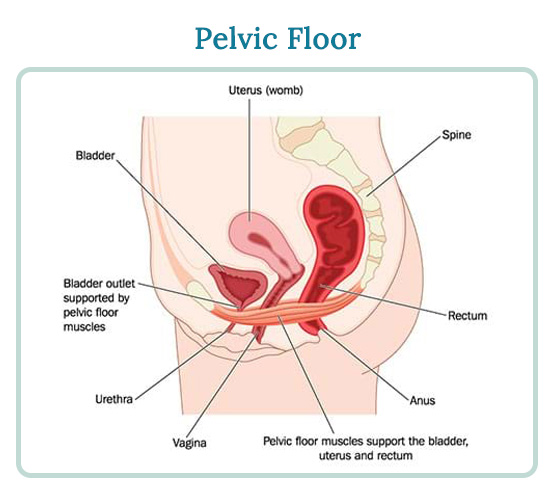
The flexibility and strength of the pelvic floor hammock come from of the way muscles and ligaments are interwoven into the bowl-like pelvic walls. These close in at the base to form the pelvic and urogenital diaphragms. A thin wall of fascia, or connective tissue, encases the pelvic floor and covers, connects, and further supports the muscles and organs of the pelvic region.
Some specifics about the structures in the pelvic floor:
- Pelvic and urogenital diaphragms: Situated at the base of the pelvic floor, both are crucial for supporting healthy childbirth and maintaining continence.
- Levators ani and the coccygeus (or ischiococcygeus): these are the muscles of the pelvic diaphragm that supports the coccyx, or tailbone.
- Pubococcygeus: one of the levators ani, this important muscle surrounds three essential openings: the bladder, vagina and rectum. When the levators ani are compromised, so are these structures.
So often, women don’t think about their pelvic floor until they have a problem. If the pelvic floor becomes overstretched, lax, or torn, it may no longer be able provide support and symptoms begin to surface.
What causes a weakened pelvic floor?
The strength of the pelvic floor can be compromised whenever its muscles, tendons, ligaments or nerves are affected by any of the following:
- Pregnancy, childbirth, episiotomy, Cesarean section
- Large uterine fibroids
- Menopause
- Hysterectomy
- Smoking and any associated chronic coughing
- Frequent straining during bowel movements
- Obesity
- Diets high in processed foods
- Inactivity that leads to decreased pelvic floor tone, strength and flexibility
Maintaining the muscle tone of the pelvic floor not only helps to control the flow of urine from the urethra, but also helps control the movement of stool from the rectum.
Pelvic floor and childbirth
Pelvic floor disorders often start during pregnancy, triggered by the weight and pressure of the fetus. There are also hormonal shifts and anatomical changes that result from giving birth, including stretching and possibly tearing or cutting of the vaginal muscles or perineum (such as an episiotomy).
A sudden, forceful push can compromise the integrity of the pelvic floor, opening up the perineum, which is connected to the pelvic floor. The skin and muscles tear from the vaginal opening down, hopefully not as far as the rectum. A torn perineum seriously compromises the pelvic floor.

Pelvic floor and sex
Strengthening your pelvic core can improve your sex life and satisfaction a lot. That’s because the pelvic floor muscles surround the vagina as well as the clitoris.
Pelvic floor strength increases stimulation during intercourse due to increased blood flow, nerve sensitivity, and circulation to the area, which results in more sensitivity to touch. Research shows women with strong vaginal muscles achieve better, longer and multiple orgasms as well as increased ability to control the timing of them.
Pelvic floor and menopause
During menopause, women experience a decrease in estrogen that can initiate thinning and weakening of the pelvic muscles and connective tissues. This makes women more susceptible to loss of tone, elasticity and suppleness in pelvic floor tissues.
As your body’s hormones fluctuate through perimenopause, pelvic floor changes can still occur whether you’ve given birth or not. For some women, proactively strengthening the pelvic muscles will help. But others may require additional support such as vaginal bioidentical estrogen.
Either way, strengthening your pelvic floor during perimenopause and menopause helps ensure comfort and pleasurable sex, while it minimizes your chances for developing urinary and/or stool incontinence later.
Pelvic floor strengthening exercises
By strengthening pelvic floor muscles, we have a good chance of avoiding tearing or prolapsing, surgery and stitches. If you wait until something happens to the pelvic floor, such as a perineal tear or a prolapse, strengthening options become more limited.
One of the best ways to start improving the strength of your pelvic floor is to practice Kegels and other exercises designed to gently stretch and tone the pelvic floor.
Kegel exercises
Kegels are highly effective and easy to do anywhere, anytime and without anyone knowing. in strengthening the pelvic floor. Here’s how to get started:
- Identify your pelvic floor muscles the next time you urinate by stopping your flow midstream to feel which muscles you will be targeting with Kegels.
- Tighten these same muscles while sitting, standing or lying down. Make sure you are isolating your pelvic floor muscles and not using your abdominal or glute muscles. This takes a little practice.
- Tighten your pelvic floor muscles for 5 seconds and then relax for 5 seconds. Repeat this exercise 10 times.
- Try to do 3 sets of 10 each day. At first, this area may feel extremely weak, or even unresponsive, but like most muscles, those in the pelvic area will respond quickly if you do Kegels regularly, and consistently.
To get even more of these toning exercises, consider trying an insertable cone or ball, available through your clinician or online. This makes it easier to focus your efforts as you progressively squeeze the muscles around your vagina, urethra, and rectum for 10 seconds, then relax for 10 seconds.
Pilates and yoga
Pilates and yoga can strengthen your core, which helps improve pelvic floor strength. The muscle groups in your core are deep within the body and include the pelvic, abdominal, back and chest muscles. These muscles attach to the spine, pelvis and scapulae and provide the foundation for every other movement you make. They also provide balance, stability, and flexibility to the rest of your body.
Pilates targets the deep core muscles with a focus on strength and flexibility. Pilates exercises can be done either on the floor with a mat or with specific equipment. Before you begin Pilates, you should talk with an instructor about any pelvic floor issues in case you need to modify some of the more intense movements.
Yoga also offers many core-strength postures specific to the pelvic floor, particularly the Root Lock, or mula bandha. (Mula means “root,” and bandha means “lock” or “bonding.”) Mula bandha is often described as an internal lift that involves the drawing the pelvic floor in and up.
While this practice isn’t hard, it’s best to work with an experienced yoga instructor who can teach you how to do the Root Lock. Like many yoga poses, the Root Lock works internal muscles while you are simply sitting comfortably on the floor. Once you learn it, you will find that the Root Lock has a lot of other body benefits beyond pelvic floor strengthening.
After you find a good yoga studio and instructor, ask about any modifications that might be needed for your situation so you can get the most from your practice. Once you’ve learned how to do the Root Lock and/or other poses, you can practice them at home on your own. For many women, the results can be impressive after only a few weeks.
Perineal massage
Massaging the perineum increases circulation to the pelvic floor to make it more supple and easier to stretch. From outside the body, the perineum is composed of the skin between the vagina and the rectum. Inside, the perineal body extends inward from the perineum and acts as an insertion point for the eight total muscles of the pelvic floor.
Perineal massage involves lubricating the thumbs and inserting them inside the bottom of the vagina and pushing down toward the back of the spine. It may feel weird at first but tolerance will increase with practice, and the pelvic floor will become more flexible. Perineal massage can be done by any woman who wants to improve pelvic floor flexibility. And it’s very effective.

Squatting
No matter how young or old you are, squatting is incredibly good for your core strength and pelvic floor. Though it seems simple, it can still be a tough position for many women.
During pregnancy, squatting not only tones the quadriceps to help them maintain that position while pushing but it also encourages the pelvic floor to stretch. Be careful to avoid straining yourself while squatting in the third trimester when the hormone relaxin loosens the ligaments in your pelvis and entire body.
Pelvic physical therapy
Pelvic physical therapy may include external and internal massage, relaxation training, strengthening work, and home exercises to gradually and steadily increase strength in the pelvic floor. Internal physical therapy can also be extremely helpful for realigning the pelvic girdle and internal pelvic floor.
If you’re having issues with your pelvic floor, you can ask your healthcare practitioner about prescribing this kind of physical therapy.
Other options to support pelvic floor strengthening
Nutrition
A diet high in protein and low in processed foods helps develop and maintain muscle tone — and even in your vagina. If you’ve had a perineal tear or episiotomy, you can eat extra protein to help the pelvic floor muscles and tissues heal more quickly by. Since it’s difficult to meet your nutritional needs every day and get enough fresh, unprocessed foods, we recommend supplementing your diet with a high-quality multivitamin/mineral supplement, such as the one we offer in our Hormonal Health Protocol.
A healthy diet can also help you find and maintain a healthy weight — that can protect your pelvic floor. Extra weight creates ongoing stress for the pelvic floor area.
Stop smoking
Women who smoke appear to be much more susceptible to pelvic floor dysfunction than those who don’t. Quitting smoking will maximize your nutrition and help prevent any chronic coughing, one of the primary triggers for pelvic floor trouble.
Biofeedback
With this technique, you work with a trained practitioner who will use electronic monitors to help you identify and tone specific pelvic floor muscles.
Feldenkrais method and Alexander technique
Though there are many differences between these two mind-body methods, both teach students to become more aware of their movements and posture. Then it’s easier to make any needed adjustments so you can move more freely, with less effort. Much of this involves how you carry your body, your spinal alignment, and core awareness. Focusing on those elements helps you overcome inflexibility, pelvic floor weakness and dysfunction more quickly. Additionally, the theory is that by teaching you to improve the way you move, you can also improve your overall sense of well-being.
Pessaries
Pessaries are removable devices used to support pelvic organs that come in a variety of sizes and shapes – diaphragm, cube, or donut. Fitted by a clinician, a pessary can be worn for weeks at a time and removed by the woman herself or the clinician for cleaning with soap and water.
Constipation prevention and treatment
To avoid straining the pelvic floor muscles and limit injury, you can take steps to prevent constipation.. Eating fresh fruits, vegetables, legumes and whole grains so you take in lots of fiber. As often as you can, skip the processed foods and sweets including white flour and white sugar. Drink plenty of water and get regular exercise. If you do get constipated, try taking magnesium glycinate at night before bed.
Estrogen
Vaginal bioidentical estrogen suppositories, available (in gels, creams or rings) by prescription from your healthcare practitioner, can help maintain vaginal tissue integrity and elasticity. It can also reduce spasms in the bladder and urethra.
You’ll be rewarded when you make time for pelvic floor strengthening
Pelvic floor function affects almost everything you do — think about today as you move around. It’s your foundation, and there is so much you can do to preserve and restore it. This is especially true during transitions like pregnancy, childbirth, perimenopause and menopause when you can support your body by building core strength. In fact, why don’t you do a round of Kegels right now?
1 Yale University Department of Obstetrics & Gynecology. 2005. Pelvic rejuvenation brochure. URL (PDF): https://www.yaleobgyn.org/urogyn/pdf/Postpartum_Brochure.pdf (accessed 06.29.2007).
2 Anderson, J., & Genadry, R. 2007. “Anatomy and Embryology,” pp. 75–85. In Berek & Novak’s Gynecology. 14th Ed. Ed. Jonathan S. Berek. Philadelphia: Lippincott, Williams & Wilkins.
Oxorn, H. 1986. Oxorn–Foote: Human Labor & Birth, 5th ed. Norwalk, CT: Appleton & Lange.
3 Wikipedia.org. 2007. Feldenkrais method. URL:https://en.wikipedia.org/wiki/Feldenkrais_method (accessed 07.18.2007).
Further reading
Alexander technique: https://www.alexandertechnique.com/at.htm
Feldenkrais Method of Somatic Education: https://www.feldenkrais.com/










