PMS is all about the symptoms it causes. According to researchers, there are more than 200 possible PMS symptoms including irritability, bloating, cramping, cravings, headaches, breast tenderness, fatigue, nausea, sleep issues and acne.

Whether you’re suffering from one painful symptom or 100, I want you to know you have the ability to change how you’re feeling from month to month. At Women’s Health Network, we’ve seen that the majority of women suffering from PMS can reduce or even prevent symptoms by addressing and resolving the root cause — hormonal imbalance.
What causes PMS symptoms?
The kinds of food you eat, the amount of essential nutrients you get every day, and the high levels of stress you regularly face are lifestyle factors that can upset hormonal balance, leading to more frequent and severe PMS symptoms. Diet and lifestyle factors are the most significant drivers of PMS symptoms but they are also the ones that are under your control.
While some monthly hormonal fluctuations are perfectly normal, others set off PMS symptoms that can range from mild to severe.
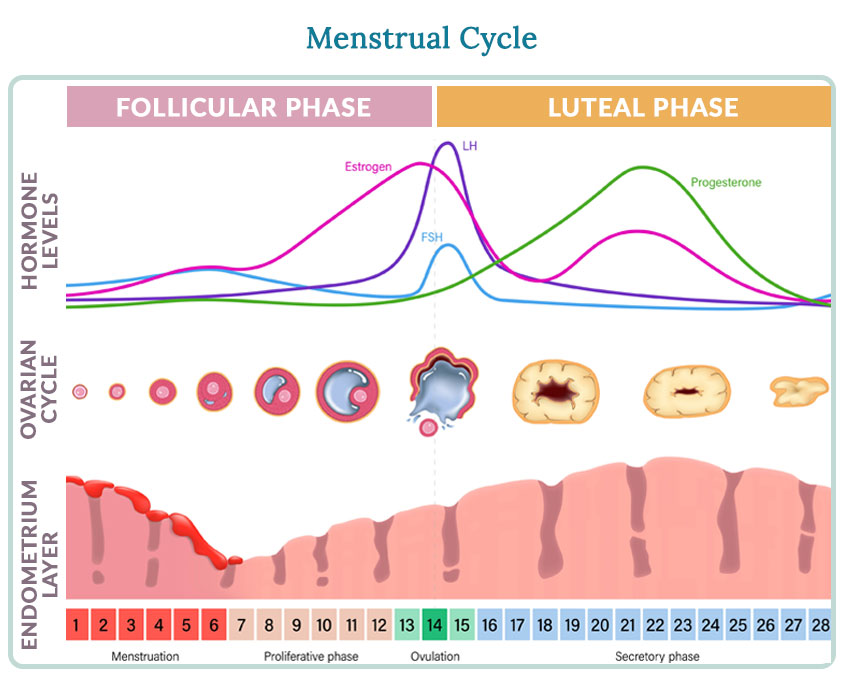
There is a natural rise and fall of estrogen and progesterone, two of our key sex hormones, during the average 28-day cycle, which can vary a few days in either direction.
But this natural rhythm of hormones is easily disrupted by a number of factors, many of which are controllable. When estrogen and progesterone become imbalanced, a variety of symptoms can arise.
How lifestyle factors drive hormonal imbalance and PMS symptoms
If you’re struggling with PMS symptoms, these are some questions to consider:
Do you have unstable blood sugar?
Unstable blood sugar causes:
- Dizziness, lightheadedness and feeling shaky
- Emotional swings
- Impatience, agitation and anger
- Uncontrollable sugar cravings (just before your period or throughout the whole month)
If you feel like your emotions and energy levels are on a rollercoaster ride because of PMS, you may be experiencing spikes and crashes in your blood sugar levels that are pushing your body into hormonal imbalance. Ups and downs in blood sugar cause their own symptoms which can exacerbate PMS.
Some women are extremely sensitive to symptom-causing fluctuations in blood sugar especially during the premenstrual period.
SOLUTION: You can reduce blood sugar highs and lows by eating regularly every few hours and including protein at each meal and snack. Eat fewer refined carbohydrates and sugary foods, especially in the lead-up to your period.
Do you have a high-stress lifestyle?
A high-stress lifestyle causes:
- Poor response to stressful situations
- Feeling on-edge, overwhelmed or out of control
- Anxiety or depression
Even though stress feels like it’s only affecting you mentally, it can have an ongoing impact on your physical hormonal balance. In one recent study, when women perceived their stress levels to be high during the early weeks of two consecutive monthly cycles, the chances of having PMS symptoms spiked up to 25 times higher!
The stress hormone cortisol can easily tip the balance of your sex hormones. Cortisol is connected to the endocrine feedback loop in your brain so it can even disrupt the way your ovaries make hormones. That’s why more stress often equals more premenstrual symptoms.
SOLUTION: Build stress relief and prevention into your life during the last two weeks of your cycle to help keep cortisol levels under control. Try regular exercise which releases tension and stress, and experiment with meditation and deep breathing for a few minutes each day.
Do you need a nutrient boost?
Lack of nutrients causes:
- Poor sleep
- Irritability
- Fatigue
- Muscle cramps
- Aches and pains
- Cravings for chocolate
Women who experience PMS symptoms may not be getting enough of specific nutrients: calcium, magnesium, and vitamins K, B6, and E. Without a daily supply of key nutrients, your body sends out an urgent signal to get your attention in the form of intensifying symptoms. As women move through life without the proper nutrition, it’s not uncommon for PMS symptoms of all kinds to escalate, often reaching a peak during perimenopause.
SOLUTION: Make sure your diet is filled with a balance of nutritious foods, with lots of vegetables, a few fruits, lean protein and whole grains. To help ward off PMS symptoms, ensure you get enough vitamins and minerals every day by supplementing with a targeted formula. Think about adding omega-3s because they have been shown to reduce many PMS symptoms, including anxiety, bloating, headache and breast tenderness.
Changing the factors that contribute to PMS
If you answered “yes” to any of the above questions, see how simple changes can make next month, and every month, more comfortable when you reduce your hormonal imbalance and PMS symptoms.
Sohrabi N, Kashanian M, Ghafoori SS, Malakouti SK. Evaluation of the effect of omega-3 fatty acids in the treatment of premenstrual syndrome: “a pilot trial”. Complement Ther Med. 2013 Jun;21(3):141-6. doi: 10.1016/j.ctim.2012.12.008. Epub 2013 Jan 16.
1 Dickerson, L., et al. 2003. Premenstrual syndrome. Am. Fam. Phys., 67 (8), 1743–1752. URL: https://www.aafp.org/afp/20030415/1743.html (accessed 10.12.2011).
2 Trout, K., et al. 2007. Menstrual cycle effects on insulin sensitivity in women with type 1 diabetes: A pilot study. Diabetes Technol Ther., 9 (2), 176–182. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/17425444 (accessed 09.20.2011).
3 Trout, K., et al. 2008. Insulin sensitivity, food intake, and cravings with premenstrual syndrome: A pilot study. J. Women’s Health (Larchmt.), 17 (4), 657–665. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/18447765 (accessed 09.20.2011).
4 Trout, K., et al. 2008.
5 Gollenberg, A. 2010. Perceived stress and severity of perimenstrual symptoms: The BioCycle Study. J. Women’s Health, 19 (5), 959-967. URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2875955/?tool=pubmed (accessed 10.12.2011).
Mann, D. 2010. Stress may raise risk of premenstrual syndrome. Study shows PMS symptoms could be more severe if women are stressed before menstruation. URL: https://women.webmd.com/pms/news/20100824/stress-may-raise-risk-of-premenstrual-syndrome (accessed 10.12.2011).
6 Wyatt, K., et al. 1999. Efficacy of vitamin B-6 in the treatment of premenstrual syndrome: Systematic review. BMJ, 318, 1375–1381. URL: https://www.bmj.com/content/318/7195/1375.full (accessed 10.12.2011).
7 Kiecolt-Glaser, J., et al. 2011. Omega-3 supplementation lowers inflammation and anxiety in medical students: A randomized controlled trial. Brain Behav. Immun. [Epub ahead of print.] URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/21784145 (accessed 09.20.2011).
Vinot, N., et al. 2011. Omega-3 fatty acids from fish oil lower anxiety, improve cognitive functions and reduce spontaneous locomotor activity in a non-human primate. PLoS One, 6 (6), e20491. URL: https://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0020491 (accessed 09.20.2011).
Ferraz, A., et al. 2011. Chronic ω-3 fatty acids supplementation promotes beneficial effects on anxiety, cognitive and depressive-like behaviors in rats subjected to a restraint stress protocol. Behav. Brain Res., 219 (1), 116-122. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/21192985 (accessed 09.20.2011).
Sampalis, F., et al. 2003. Evaluation of the effects of Neptune Krill Oil on the management of premenstrual syndrome and dysmenorrhea. Altern. Med. Rev., 8 (2), 171-179. URL (PDF): https://www.altmedrev.com/publications/8/2/171.pdf (accessed 09.20.2011).
8 van Die, M. 2009. Effects of a combination of Hypericum perforatum and Vitex agnus-castus on PMS-like symptoms in late-perimenopausal women: Findings from a subpopulation analysis. J. Altern. Complement. Med., 15 (9), 1045–1048. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/19757982 (accessed 09.20.2011).
9 Whelan, A., et al. 2009. Herbs, vitamins and minerals in the treatment of premenstrual syndrome: A systematic review. Can. J. Clin. Pharmacol., 16 (3), e407-429. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/19923637 (accessed 09.20.2011).
Thys-Jacobs, S., et al. 1989. Calcium supplementation in premenstrual syndrome: A randomized crossover trial. J. Gen. Intern. Med., 4 (3), 183–189. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/2656936 (accessed 09.20.2011).
Thys-Jacobs, S., et al. 1998. Calcium carbonate and the premenstrual syndrome: Effects on premenstrual and menstrual symptoms. Premenstrual Syndrome Study Group. Am. J. Obstet. Gynecol., 179 (2), 444–452. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/9731851 (accessed 09.20.2011).
10 Khine, K., et al. 2006. Magnesium (Mg) retention and mood effects after intravenous Mg infusion in premenstrual dysphoric disorder. Biol. Psychiatry, 59 (4), 327–333. URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1509101/?tool=pubmed (accessed 09.20.2011).
Walker, A., et al. 1998. Magnesium supplementation alleviates premenstrual symptoms of fluid retention. J. Women’s Health, 7 (9), 1157–1165. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/9861593 (accessed 09.20.2011).
Facchinetti, F., et al. 1991. Oral magnesium successfully relieves premenstrual mood changes. Obstet. Gynecol., 78, 177–181. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/2067759 (accessed 09.20.2011).









