Reviewed by Dr. Sharon Stills, NMD
PCOS (Polycystic Ovary Syndrome) is a hormonal disorder that affects women of reproductive age. It is characterized by a range of symptoms related to hormonal imbalance and disrupted ovulation.
Women with PCOS don’t usually have the exact same symptoms but nearly all of them have one thing in common: insulin resistance. At the same time, insulin resistance is just one player in the complex mix of hormonal imbalances that lead to PCOS. And the ways these imbalances show up can vary widely. That’s one of the big reasons why it’s often so challenging to trace the range of symptoms back to their root cause: PCOS.

Every woman with PCOS has travelled a separate path to her diagnosis, but all can benefit from knowing more about what’s going on in their bodies. Understanding how PCOS develops can help you figure out how to make specific changes to your diet and lifestyle that will reduce your PCOS symptoms.
Table Of Contents:
Symptoms of PCOS
As with most “syndromes,” PCOS shows up differently in each woman. Every woman with PCOS has a symptom picture that will change during the course of her lifetime, too. Some women experience very few symptoms, while others have many. High androgens may cause acne, male-pattern hair growth or hair loss, or other visible changes.
The wide range of PCOS signs and symptoms includes:
- Irregular or absent periods
- Infrequent (or total lack of) ovulation
- Infertility
- Unwanted hair growth
- Hair loss and male pattern baldness
- Hirsutism and male pattern hair growth (facial hair, etc.)
- Acne
- Darkened skin patches
- Mid-section weight gain (apple shape)
- Cravings
- Anxiety
- Depression
- Cystic ovaries (not all women with PCOS develop ovary cysts)
Of all the health concerns caused by PCOS, insulin resistance, irregular periods and unwanted weight gain are the ones women most often want help with.
Here’s how these three problems can play out in women with PCOS:
Irregular or absent periods. With PCOS, you may go for months without a period. Or you may have difficult periods, bleeding heavily for days — or weeks. Heavy bleeding occurs when the body naturally sheds the uterine lining but the lining has gotten extra thick. Also, during periods — even regular periods — the ovary may or may not have released an egg. This unpredictability can be very disturbing, especially if a woman is trying to become pregnant. PCOS is one of the major causes of infertility in women, affecting between 4% and 18% of women of childbearing age.
Unwanted weight gain. Extra fat cells fuel production of extra estrogen, which further disrupts ovulation. This extra fat usually accumulates around the waist — where it can be more difficult to lose, even with diet restriction and exercise. This stubborn extra weight is more likely to have adverse long-term effects on your health, including cardiovascular disease.
Insulin resistance. Insulin resistance is common in women with PCOS, which can lead to elevated insulin levels, fatigue after eating, and an increased risk of developing type 2 diabetes.
It’s fairly common for less obvious clues to PCOS to be missed. For example, polycystic ovaries (PCO) can occur even with normal periods and normal androgen levels, or they may come and go. And some women with PCOS do not have cysts at all. Hormonal imbalance is variable and dynamic and so its signs and symptoms are, too. This is why diagnostic criteria for PCOS are open to interpretation, and why appropriate diagnosis and treatment are often delayed.
What causes polycystic ovary syndrome (PCOS)?
Women with PCOS typically deal with the following three-factor hormonal scenario:
1. High amounts of androgens (including testosterone)
2. Insulin resistance (impaired sugar tolerance)
3. Both of the above interacting in a positive feedback loop with one amplifying the other
Genetics, environment and lifestyle are some of the major factors that can influence these different hormonal scenarios.
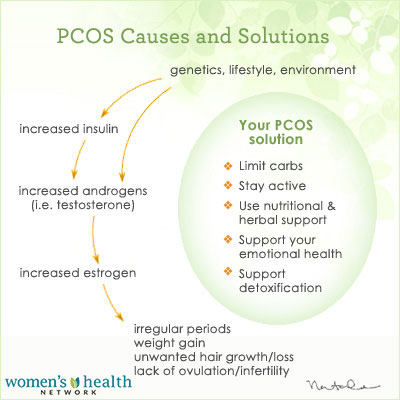
This is a simplified diagram of the chain of events often leading to PCOS. The good news is that limiting your carbs and taking other lifestyle measures can make a big difference.
PCOS sufferers typically have:
Increased insulin. The majority of women with PCOS need to first address an overproduction of insulin (hyperinsulinemia), which, overtime, leads to insulin resistance, but also stimulates the production of androgens. Androgens are sex hormones, like testosterone, that are usually considered “male” hormones. It’s thought that circulating insulin may be one of the factors that confuse the ovaries, because when it’s reduced, the ovaries often function better. There is a much smaller group of women with PCOS who are not insulin resistant though research suggests that that they still produce excess androgens. It’s still not clear why this happens.
Increased androgens. Excess androgens in women with PCOS disrupt overall hormonal balance and produce some of the syndrome’s characteristic signs. It’s normal for all women to have some androgens, but excessive amounts can lead to weird hair growth, or hair loss in “male” patterns (facial hair and/or male pattern baldness).
Increased estrogen. Excess androgens can also be converted into estrogen. This extra estrogen suppresses the normal surge in follicle-stimulating hormones (FSH) that triggers ovulation. When this happens, ovulation generally doesn’t occur, which elevates luteinizing hormone (LH) and leads to low progesterone. Without enough progesterone, the body can’t fully support normal ovulation or pregnancy.
Irregular/absent periods and cyst formation. Many women with PCOS have irregular periods or stop menstruating altogether. If ovaries produce an abundance of egg follicles each month, but do not release an egg, a series of small cysts forms that often look like a string of pearls. This is where the name “polycystic” ovarian syndrome comes from: “poly” = many.
How is PCOS treated?
Fortunately, there are a lot of natural ways to take care your body if you have PCOS — like taking steps to support better hormonal health, changing your diet, and adjusting a few lifestyle factors. If you suspect you might have PCOS, the sooner you recognize your symptoms for what they are, the better.
Here are some natural PCOS treatment approaches that can help:
Moran, L., & Teede, H. 2009.
2 Legro, R., et al. 2004. Detecting insulin resistance in polycystic ovary syndrome: Purposes and pitfalls. Obstet. Gynecol. Surv., 59 (2), 141-154. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/14752302
3WebMD. 2011. Polycystic ovary syndrome (PCOS) — symptoms. URL: https://women.webmd.com/tc/polycystic-ovary-syndrome-pcos-symptoms
4Halperin, I., et al. 2010. The association between the combined oral contraceptive pill and insulin resistance, dysglycemia and dyslipidemia in women with polycystic ovary syndrome: A systematic review and meta-analysis of observational studies. Hum. Reprod., 26 (1), 91-201. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/21059754
5 March, W., et al. 2010. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum. Reprod., 25 (2), 544-551.
Lukaczer, D. 2005. The epidemic of insulin insensitivity. In Textbook of Functional Medicine, ed. D. Jones & S. Quinn, 247. Gig Harbor, WA: Institute for Functional Medicine.
Azziz, et al. 2004. The prevalence and features of the polycystic ovary syndrome in an unselected population. J. Clin. Endocrinol. Metab., 89 (6), 2745-2749. URL: https://jcem.endojournals.org/content/89/6/2745.full (accessed 05.18.2011).
Sheehan, M. 2004. Polycystic ovarian syndrome: Diagnosis and management. Clin. Med. Res., 2 (1), 13-27. URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1069067/?tool=pubmed
Asunción, M., et al. 2000. A prospective study of the prevalence of the polycystic ovary syndrome in unselected Caucasian women from Spain. J. Clin. Endocrinol. Metab., 85 (7), 2434-2438. URL: https://jcem.endojournals.org/content/85/7/2434.full.
Nestler, J. 1999. Chapter 19. Insulin resistance effects on sex hormones and ovulation in the polycystic ovarian syndrome. In Insulin Resistance: The Metabolic Syndrome X (Contemporary Endocrinology), 347. G. Reaven & A. Laws, eds. Totawa NJ: Humana Press, Inc.
Diamanti-Kandarakis, E., et al. 1999. A survey of the polycystic ovary syndrome in the Greek island of Lesbos: Hormonal and metabolic profile. J. Clin. Endocrinol. Metab., 84 (11), 4006-4011. URL: https://jcem.endojournals.org/content/84/11/4006.full (accessed 05.18.2011).
Knochenhauer, E., et al. 1998. Prevalence of the polycystic ovary syndrome in unselected black and white women of the southeastern United States: A prospective study. J. Clin. Endocrinol. Metab., 83, 3078-3082. URL: https://jcem.endojournals.org/content/83/9/3078.full (accessed 05.18.2011).
6 García-Romero, G., & Escobar-Morreale, H. 2006. Hyperandrogenism, insulin resistance and hyperinsulinemia as cardiovascular risk factors in diabetes mellitus. Curr. Diabetes Rev., 2 (1), 39-49. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/18220616 (accessed 05.17.2011).
7 García-Romero, G., & Escobar-Morreale, H. 2006.
8 Koiou, E., et al. 2011.
Li, X., & Lin, J. 2005. [Clinical features, hormonal profile, and metabolic abnormalities of obese women with obese polycystic ovary syndrome]. Zhonghua Yi Xue Za Zhi, 85 (46), 3266–3271. URL (abstract): https://www.ncbi.nlm.nih.gov/pubmed/16409817 (accessed 05.18.2011).










