Your bone health - what every woman needs to know to build strong bones for life
Reviewed by Dr. Susan E. Brown, PhD
Women don’t usually get all the information they need to understand what is happening to their bone health — even from their doctors. That makes it hard for them to make the best decisions for their long-term bone health.

This “knowledge gap” is built into our medical system. So, let’s give you an overview of what you do need to know and then turn to the crucial question: what can I do to restore my bone health?
Table of contents:
- The osteoporosis epidemic among women
- Your bone health is a bigger issue than osteoporosis
- The natural approach to bone health
- What does bone health mean for you?
- The problem with conventional treatment for bone loss and osteoporosis
The osteoporosis epidemic among women
According to the U.S. Centers for Disease Control and Prevention, 25% of American women over 65 have osteoporosis — almost 7 million women. That’s an incredible figure. And it’s a big increase from prior generations. Importantly, women are four times more likely than men to suffer excessive bone loss and osteoporosis. Why?
While bone loss and replacement is normal, as women age, the rate of bone loss usually outstrips replacement. And about 20% of a woman’s lifetime bone loss happens in menopause.
It’s a little-known fact that bones aren’t just there to hold up our muscles and organs — they’re also closely involved in many of our other body systems. Blood cells are born in bone marrow, for instance, and bone has a dynamic relationship with hormones such as estrogen, insulin, and cortisol, among others. Estrogen and insulin are protective of bones, while cortisol and other stress hormones are destructive of bone. What this suggests to us is that whenever you’re experiencing a hormonal imbalance, it is often harmful to your bones and disruptive of normal bone formation.
It’s no coincidence that the rise in osteoporosis and poor bone health is happening just as hormonal disorders affecting women are also at epidemic proportions.
Bone health risk factors
- Hormonal imbalance
- Low bone density
- pH imbalance
- Inactivity
- Insufficient nutrition
- Dietary excesses
- Indoor lifestyle
- Digestive issues
- Family history
- Previous fracture
- Low body weight
- Emotions and stress
- Toxins
- Smoking
- Inflammation
- Medications
- Diseases
How modern life creates bone loss
We need to understand bone loss in the context of how modern life affects our bodies. Bones are not static, like a masonry wall. They’re alive, more like a coral reef, constantly being broken down at a cellular level (resorption) and rebuilt (formation).
Resorption and formation represent a complex process that has evolved over millions of years to require two key components: exercise — especially weight-bearing exercise — and the presence of certain key nutrients in our food. But in modern life, how much exercise we get (compared to how much we need) and the types of foods we eat have radically changed.
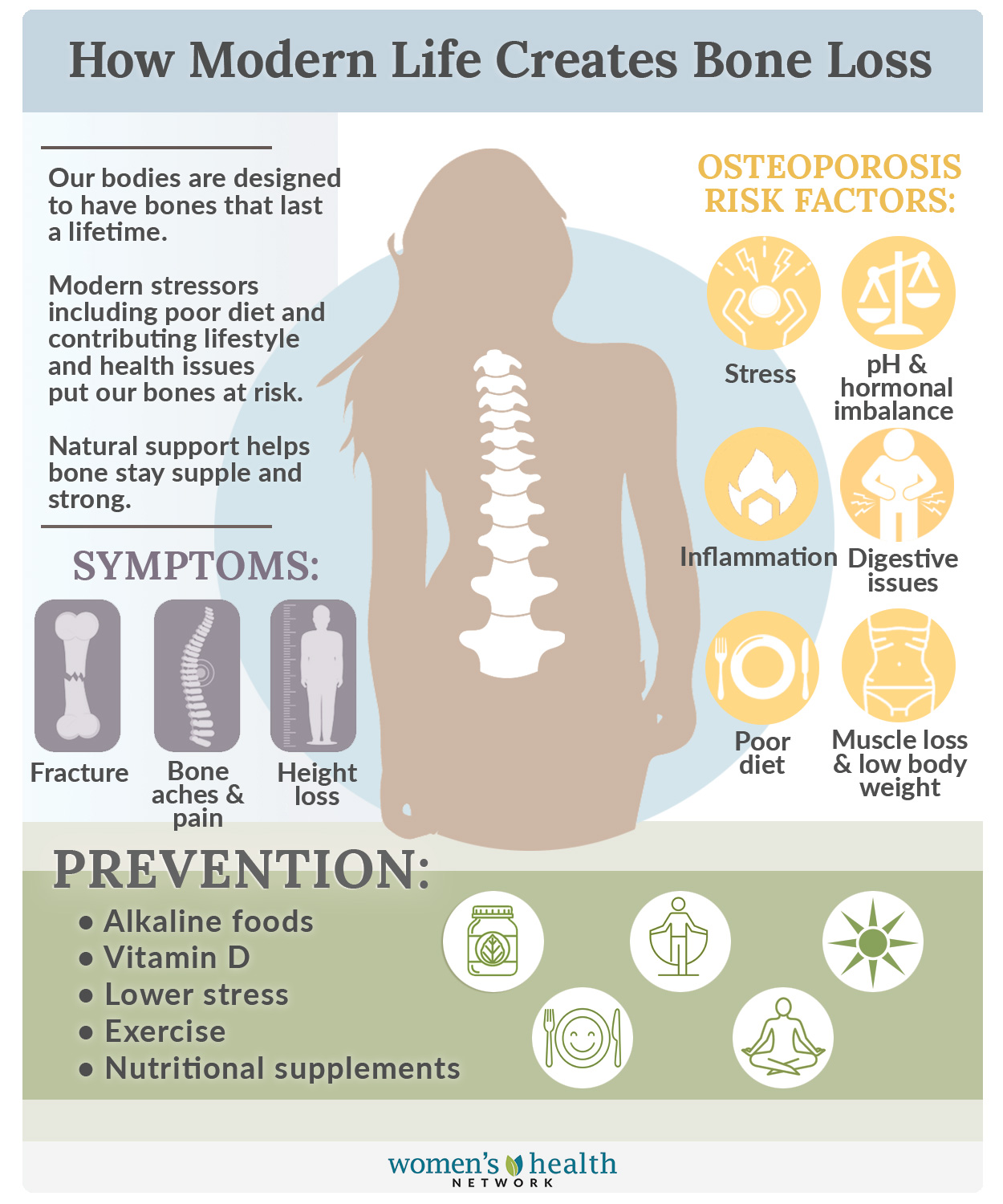
The bone-building power of exercise — something our sedentary lifestyle is missing
Our bones respond to physical stress by building bone. If we lift weights —whether bags of food, or babies, or weights at the gym — our bodies respond by putting extra bone-building effort into the skeletal parts stressed by those weights. Hopping, jumping and simply walking are other load-bearing exercises that trigger bone building. But if we don’t exercise…we don’t build bone as much. Modern life has led us to become sedentary and to do much less physical work — and that’s a big reason why there’s been such a noticeable increase in osteoporosis.
Nutrients – Women aren’t getting the nutrients their bones require
And then there’s nutrition. If you think about how our grandmothers ate, you realize there’s a radical difference in how food gets from the farm to the table. As recently as the 1950s and 1960s, people still made food at home from fresh, local (and sometimes home-grown) ingredients rather than buying it packaged or pre-made.

Compare that to how most Americans eat now — fast food loaded with salt and sugar, or canned and frozen meals leached of most nutrients — and you start to realize that we’re losing out on a lot of nutrients that were available to prior generations. But it doesn’t stop there: Because of intensive, industrial agriculture, our crops grow because they are artificially stimulated, not because their soil is rich with mineral and nutrient value. Our ancestors could eat the “right” foods and get enough of the key nutrients bones require. But if the minerals aren’t in the soil, they aren’t in our food. The following chart shows how some nutrients levels have dropped in common fruits and vegetables over the past several decades:
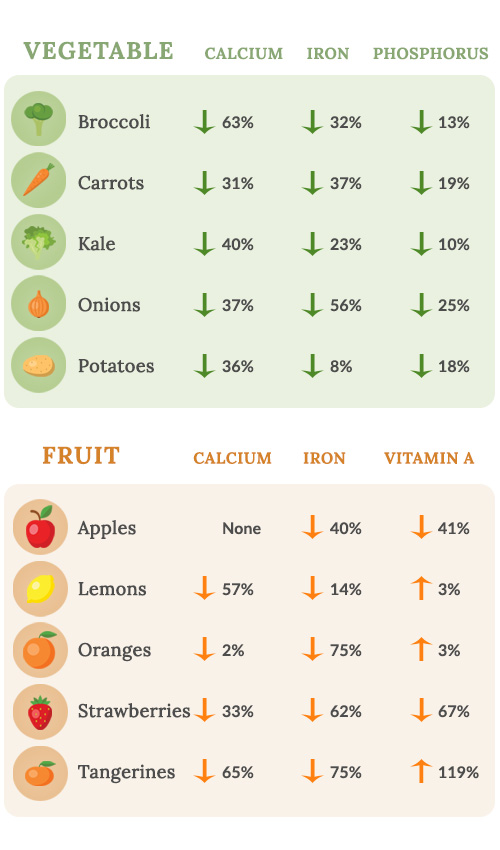
What this means is, our bones aren’t getting enough of these key inputs to keep them strong; women need a high quality bone supplement to make up the dietary gaps. At the same time, women are also being hit with greater and greater demands. For example, bones help maintain a stable pH in our blood. If our internal pH becomes too acidic, the body literally dissolves our bones to provide the alkaline minerals (such as calcium and potassium) needed to restore pH balance. And modern life is full of factors adding to the acid load — sugar, for one (it’s acid-forming) but also stress, whether emotional or physical. Did your doctor ever tell you that?
One source of stress, ironically, may be added into your diet just as you try to eat “better” — pesticides and similar toxins found in conventionally grown fruits and vegetables can play havoc with bone health. Many are endocrine disruptors. This means they act like hormones in the body, which interferes with your real hormones. Other toxins become embedded in bone, changing its very nature, and/or disrupt the metabolic pathways involved in absorption and formation.
The picture is clear: without informed action, most women are going to experience impaired bone health. So it’s no surprise that that’s exactly what’s happening.
But what can you do about these problems to protect yourself and your loved ones?
The American medical system’s typical answer to such questions amounts to “better living through chemistry” — if there’s a health issue, there’s a drug for it. The problem is, bone drugs are oversold. The drugs don’t help as much as promised, they aren’t universally effective, the side effects are generally worse than predicted, your doctor doesn’t take enough time describing the negative side effects, and the system conceals those side effects, even from your doctor.
And you’re rarely told about natural alternatives.
Your bone health is a bigger issue than osteoporosis
The biggest worry most women have related to osteoporosis is a bone fracture — and there’s good reason for concern. Osteoporosis is also associated with balance, falls, and broken bones, which are also critical events in older women. If a woman over 65 breaks her hip in a fall, there is a 50% chance she will die within the year. But bone health is also strongly correlated with frailty and mobility, and closely predicts how long women can remain self-sufficient and live independently and take care of themselves.
Osteoporosis and osteopenia (commonly defined as a precursor to osteoporosis) are also associated with many other serious health issues, including diabetes, hyperthyroidism, asthma, celiac disease, lupus, depression and dementia. This doesn’t mean that osteoporosis causes these diseases — or vice versa — but bone health is closely tied to overall health in ways that science doesn’t yet fully understand, and the steps you take to care for your bones often has benefits for other conditions, too.
All this means that your bone health is crucial, and every woman should devote attention to hers. What it doesn’t mean is that you have to accept the conventional medical “wisdom” that there are just two choices: Bone drugs or fractures. You don’t have to give into fear over all those scary statistics! There is another, better way.
You can have better bone health — without drugs or side effects
Our approach to women’s bone health is based on something I learned as a medical anthropologist: that women from certain countries almost never experienced osteoporosis. It led me to wonder, what was different about them? My research showed that the chief factors were that the women did lots of physical labor, they ate an alkaline diet rich in key nutrients, their environment was mostly clear of toxins, and their lives were largely free of chronic stress.
Over the past 30 years, I have explored how those factors influence bone building and bone loss. My research has led me to develop protocols for women so they can strengthen and support their bones at every stage of bone health — whether they are already diagnosed with osteoporosis, have broken a bone, or are just starting to notice signs of bone loss in menopause.
I also developed a model for assessing fracture risk — a key way to measure your bone health.

The natural approach to bone health
My Better Bones approach to bone health is simple: focus on the bone health risk factors that contribute to bone loss and take steps to offset them, not with drugs, but with changes to your diet and lifestyle and using a high quality bone health supplement to encourage the body’s natural bone-building processes to kick in.
Start with an individual assessment
It starts by examining the specific factors in your life that could be impacting your bones. Are you losing bone? How fast? And are there specific issues in your health that may be accelerating bone loss, be it menopause, nutritional deficits, low Vitamin D, or a hidden health problem putting strain on your body’s balance?
In some cases, these factors can be readily identified by completing my fracture risk assessment — but for others, medical tests may be needed to uncover hidden physiological issues causing bone loss and excessive bone breakdown, such as diabetes, celiac disease, or other silent health problems.
Diet and nutrition
Next, we look at your diet. Are you following an alkaline diet and eating foods rich in bone-building nutrients, or are your diet and food choices skewed toward processed foods high in carbohydrates? What steps can you take to make sure you’re getting the full range of nutrients your bones need — calcium and Vitamin D and many more!
Supplementation
What kind of bone health supplements are your best match? In situations where you have significant nutrient gaps or special nutritional needs, supplementation may be required. Look for natural supplements that deliver intensive supplemental nutrition for bones with therapeutic amounts of key nutrients for strengthening and rebuilding bone. If your supplementation needs are more moderate, a quality daily support supplement for bone health can maintain a constant supply of bone-building vitamins and minerals.
Digestion
Another key factor to assess is, how well is your digestive system working? For many people, especially those eating the standard American diet (known as “SAD”), which is high in processed foods and full of animal fats and carbohydrates, the digestive tract isn’t operating to its optimal level. Restoring balance to the intestinal microflora by taking a high quality probiotic and eliminating sources of inflammation and poor absorption is vital to making sure the nutrients you need get in — while toxins and pathogens don’t.
Exercise
There’s one factor that almost everyone needs to rethink, and that’s exercising for bone health — because even fit people lose bone if they’re focused only on aerobic exercise or weight loss. Strength training and other methods of challenging bone and muscle to increase capacity is a must for bone health — and even a little each day goes a long way!
State of mind
And last but not least, we address the habits of mind that can directly damage bone — stress, worry, anxiety, and other negative mental states. Very few medical practitioners understand that the body’s first response to stress is to destroy bone in order to support the flight-or-fight response.
The Better Bones approach understands that bringing peace and tranquility to our thoughts is crucial to halting bone loss and promoting greater health, not just in the bones, but in the whole body.
What does bone health mean for you?
For most women, the need to build and maintain strong bones isn’t a huge priority when they’re young. But as they approach menopause, that starts to change — maybe their mother or other close relative has osteoporosis, or they’ve learned that women lose bone during menopause. Or they may have fractured a bone or been told they have osteopenia by their healthcare provider, either of which can be a shocking wake-up call. But in all these scenarios, the doctor’s response is never to ask, How did this happen?
Instead, the conventional response is, Which bone drug should you take?
There are three main reasons why conventional medicine is so drug focused:
- Conventional medical care tends to regard thinning bones — whether related to menopause or some other cause — as a chronic disease, one requiring long-term management, but something that can’t really be “cured” even if it can be slowed. You can find out right now why thinning bone alone isn’t a good predictor of fracture risk.
- Conventional doctors are primed to recommend drug therapy as their “go-to” solution. They are either uninformed about natural alternatives for bone health, which studies have shown to be as effective as or even more effective than conventional medications for bones, or else they don’t believe their patients will make the necessary lifestyle changes to get good results — so they don’t mention them at all. This is unfortunate, since so many bone health problems can be effectively resolved using natural solutions.
- There’s tremendous misinformation in the general conversation about bone health and osteoporosis. Much of the advice available online, in the media, and even from healthcare practitioners is fear-based, leading women to feel helpless in the face of bone loss, and concerned that they will have a life-changing fracture, even if in reality they’re not really at great risk. (This is also true in other areas of bone health, such as joint pain and arthritis, or hip or knee replacement, where similar misinformation abounds.)

The problems with conventional treatments for bone loss and osteoporosis
In our great-grandmother’s day, osteoporosis was diagnosed when an older woman broke a bone for no good reason. Back then, we had no way to diagnose bone health except for that outcome. But it didn’t matter much because such fractures were rare.
HRT for osteoporosis is risky business
As osteoporosis became more common, researchers explored why that might be— and recognized a clear correlation between the decline of hormones in menopause and bone loss. They not unreasonably inferred that losing estrogen was the cause of bone loss and proposed that hormone replacement therapy (HRT) using synthetic estrogen would protect women’s bones as they aged (and would make them stay youthful and sexy, too, which was a great marketing tool). HRT’s side effects would only become clear decades later after independent, government-funded research. But with concerns about increased risk of breast cancer being raised in the 1970s and 1980s, the pharmaceutical industry started looking for an alternative treatment for osteoporosis.
Bone density doesn’t tell the whole story
Coincidentally, at about that time (1987), DEXA (dual-energy x-ray absorptiometry) scanning was introduced. Physicians could now see how dense the bone tissue was, and armed with this tool, a consensus emerged among doctors that denser bone was stronger bone — even though there was no evidence to prove that bone density should be equated with bone health.
Based on this belief, pharmaceutical companies began looking for ways to increase bone density. In 1995, the first bisphosphonate bone drug, Fosamax, was introduced. Fosamax increased bone density by slowing bone resorption. Now that they had a drug, bone density became even more popular with doctors as a measure of bone health, and prescriptions for the new bone drug grew rapidly—so rapidly that it became a business model.
Creating a new diagnosis to fit the prescription
Pharma companies introducing bisphosphonates or other drugs for osteoporosis persuaded the medical profession to endorse the creation of a new diagnosis, osteopenia, based on a loss of a certain percentage of bone density compared to a 21-year-old woman. There was no proof this threshold was predictive of osteoporosis, nor that this threshold of bone loss was abnormal for women of any given age. (Why shouldn’t a 65-year-old woman have a lot less bone density than a 21-year-old?) But overnight, the market for bone drugs was many times larger. Not good medicine, but very good business! By the way, NPR has a great segment on this controversy which I encourage you to give a listen. You will also find osteopenia making the cut as one of my top myths about bone health!
The conventional system is designed for profits, not women’s health

And this is where we stand today: Women’s bone health is shaped by business forces more than by medicine. The standard of care (i.e. the treatment protocols approved by the medical profession and insurance companies) is designed to funnel them toward medical interventions that aren’t necessarily helpful to the individual woman, but that offer wonderful profitability for the companies that make them. That may sound like a political statement, but it’s necessary to understand why “the system” isn’t going to meet your bone health needs in the way that’s best for you.
Doctors today recommend the DEXA scan for all women over 65 with “moderate risk of fracture” who are not already on bone drugs, and for younger women if they have health factors that contribute to fracture risk. We probably have better measures of bone health than the DEXA test, but there is little support in the medical profession to move off the standard of bone-density testing.

We’ve also learned more about the dangers of bone drugs in recent years, though the drug industry disputes the most adverse findings. As with the 60-year history of HRT, the real risks of bisphosphonates are only being revealed in independent research, not the drug industry’s own reported findings. This emerging science shows an ever-expanding web of side effects, from necrosis of the jaw to hormonal disorders to increased dementia. We have to wonder whether some of the many diseases associated with osteoporosis are actually effects of the drugs widely given to treat it, rather than being consequences of the disease itself.
Drug companies defend themselves against these critiques by arguing that although there may be serious side effects, they are worth the risk — because, in their narrative, the only alternative is a broken hip or other life-threatening fracture. But they have a vested interest in convincing women that these are the only options available — and fortunately for us, they aren’t!
The natural approach to bone health is waiting for you

My goal is to give women the information they’re missing, so they can make the best decisions for themselves — and hopefully reach the best outcomes too! Bone health problems are a wake-up call that women can use to transform their overall health and give their bones targeted support so they can build strong bones for life — and the only side effects will be more energy, vitality, longevity, and enjoyment of life.
We have a lot of information to share with you. Take heart and take action!











